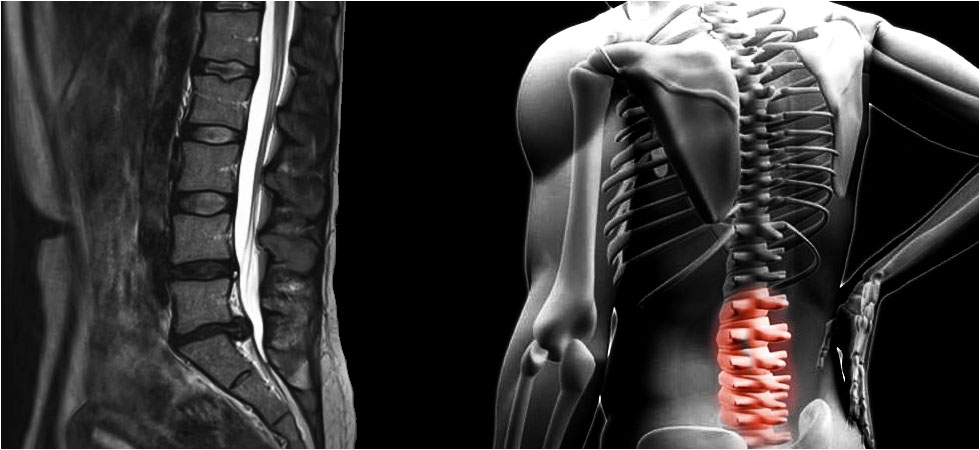
Most commonly associated with sports injuries, Orthobiologics are biological substances, such as platelet-rich plasma (PRP) or stem cells. These substances are used to speed the healing process for musculoskeletal injuries.
They may be used alone or in combination with conventional pharmaceutical and non-pharmaceutical based treatment. More specifically, orthobiologic therapies introduce high concentrations of naturally occurring cellular concentrates to an injury with the intention of expediting the healing of muscles, ligaments, tendons, and bones; thereby shortening recovery time and decreasing injury-related inflammation and pain.
In sports medicine, orthobiologic treatments are used to treat both acute and chronic conditions, including common conditions caused by overuse.
Athletes and orthopedists often turn to orthobiologic therapies in the hope of returning an athlete to preinjury physical condition as soon as possible. For the most part, orthopedists will use biologics in place of pharmaceuticals and/or invasive surgery.