What is regenerative medicine?
Regenerative medicine is the exciting cutting-edge “medicine of the future” which holds the hope & the promise of efficacy which revolves around the ability of human tissue to be repaired, replaced, and healed (regenerated) once human tissues and organs are damaged or diseased. Regenerative therapies aid and supplement the natural healing mechanisms of the body. These therapies often employ the activation of stem cells to stimulate renewal of tissue damaged by injury, disease, or age. The rapid expansion of scientific knowledge offers great promise for continuing advances in this field of medicine which holds vast potential to improve the quality of human life.
What are stem cells?
Stem cells are the basic building blocks of life. They are unspecialized cells that can produce more stem cells through mitosis or differentiate into specialized cells that carry out specific functions in the body. Stem cells are found throughout the body’s tissues, organs, and systems although usually in small quantities in adults.
What are hematopoietic stem cells?
Hematopoietic stem cells (HSCs) can give rise to all types of blood cells including red blood cells, white blood cells, and platelets. They are particularly useful in the treatment of blood-related diseases and conditions.
What are mesenchymal stem cells?
Mesenchymal Stem Cells (MSCs) are multipotent stromal cells that are non-blood forming stem cells and can differentiate into a variety of cell types including muscle, bone, cartilage, and fat cells.
When introduced into a patient’s body, MSCs can repair or replace damaged or degenerating tissue by communicating with the surrounding cells thus causing a cellular cascade of healing (paracrine signaling).
Historically, the term MSC was coined in the late 80’s by the biomedical research authority, Dr. Arnold Caplan of Case Western Reserve. The acronym has recently been redefined by Caplan to “Medicinal Signaling Cell” since these cells secrete powerful bioactive molecules involved in cellular signaling and regeneration. Caplan now describes MSCs as a “multisite-regulatory dispensary” (Natural Drug Store).
The production of MSCs in the human body, can be precipitated by bioactive placental tissues containing Growth Factors, Cytokins and other powerful bioactive agents which trigger cell signaling.
The remarkable ability of MSCs make them irreplaceable in medical treatments.
What are accessible sources of stem cells?
Stem cells can be extracted from various parts of the body. They have been extracted from bone marrow and adipose tissue for a few decades. More recently, birth tissues from live births, including umbilical cord blood, cord tissue, with Wharton’s Jelly, and amniotic membrane tissue, have been found to be a rich source of both HSCs and MSCs and in addition, precipitate target tissue production of MSCs through paracrine signaling. Growth Factors, Cytokins, Exosomes & micro-RNA from birth tissues give rise to Stem cells in this way. These cells, as well as MSCs contained in Wharton’s Jelly tend to be more fit than stem cells obtained from adult stem cells.
WHARTON’S JELLY
Wharton’s jelly is a gelatinous substance found in the umbilical cord which is rich in stem cells. Studies have shown that mesenchymal stem cells (MSCs) have low immunogenicity. Human umbilical cord Wharton’s jelly provides a new source for MSCs that are highly proliferative and have multi-differentiation potential. Wharton’s Jelly Cells (WJCs) express MSC markers but low levels of human leukocyte antigen (HLA)-ABC and no HLA-DR. WJCs have low functional immunogenicity and therefore recipient rejection has not been documented.
Advanced Regenerative Medicine
Advanced Regenerative Medicine involves the use of regenerative biomolecules, tissue engineering and stem cells to treat diseased or injured tissues.
- Published in Corporate News / Blog
Controlling Stem Cells…through their environment
We want to talk here about the fascination that stem cells produce over scientists and lay people. Ever since we heard about this microscopic buddies for the first time, we started imagining endless possibilities for treatments and, why not: cures.
So scientists went right to work. One of the objectives was to find ways to control how stems cells develop into other cell types, in the hopes of creating new therapies. The work is on its infancy but, as we all hear constantly, it is very promising.
Researchers have learned that pluripotent cells—stem cells that have the ability to differentiate into any kind of cell- when cultured in certain types of confined spaces started activating genes that determined the tissue those cells were going to become. Most of the medical investigation on stem cells has focused on modifying the combination of growth solutions to stimulate differentiation. The cellular surroundings are an important element to controlling how stem cells transform into other cell types. The research continues. and the perspectives are exciting. We have already obtained dopamine producing neurons from pluripotent cells! We have already created a sugar based scaffold of blood vessels!!
Now what happens out of the lab?. Physicians and patients alike have embraced the use of fresh adult stem cells obtained from fat or bone marrow to treat some degenerative conditions. Clinical trials have demonstrated significant improvement, for example in knee osteoarthritis, sports injuries, frozen shoulder etc. What happens in this case? how do these cells work?. Well: adult stem cells not necessarily differentiate or “become” cartilage, or tendon, or muscle. By the release of information, proteins, anti-inflamatory elements; this cells will influence the environment and stimulate the growth and differentiation of the local cells, hence regenerating and healing damaged tissue. So with slight differences what is being achieved in the laboratory, happens in a very natural fashion inside our bodies through the harnessing of our own cells healing power!
Isn’t it all short of amazing?
Will see you in the next blog. Keep your cells healthy!
- Published in Corporate News / Blog
Photobiomodulation and why do we use a LED to irradiate PRP
So we have been in the regenerative medicine specialty for about 8 years. Just like pretty much everyone, we started by using Platelet Rich Plasma. We learnt about it, we were fascinated by it and we treated our patients with it. Patients loved and so did we. ‘
PRP, if obtained and used correctly is a very powerful tool to implement in any medical practice. Especially if we deal with the elderly, osteoarthritis, wear and tear of tendons and ligaments, loss of vitality. The PRP is also very frequently used in Plastic and reconstructive surgery. For wound care, scar improvement and overall rejuvenation of the skin.
But why does it work? and how?
Well, we are all familiar with platelets. They seem to have significant power and influence over tissue regeneration, and by concentrating them in a blood sample we can obtain signaling proteins, cytokines and growth factors. If we add white blood cells to the mix, we will have what is called L-PRP (leukocyte rich PRP), which makes that “soup” even more interesting.
Now, to harness the power of those bioactive substances we need to coax the cells into releasing them. Normally the platelets get activated by the addition of calcium, or by contact with collagen. But several studies have demonstrated the influence of laser of low intensity over the activity of some cells. That effect is called “Photobiomodulation”. Basically it is form of light this modality uses non-ionizing light sources, like LEDs or Helium-Neon lasers to produce photochemical events at various biological scales. It have been demonstrated that this light will react with the enzyme Cytochrome C oxidase which is paramount in the mitocondrial processes.
Several scientists went on to study this light and its effects over cellular cultures. and they found that cells proliferate more when exposed to low level laser, they also showed increased viability!
So we went on to compare the levels of cytokines and growth factors in an irradiated sample and a non irradiated one. And sure enough some of the growth factors even tripled the concentrations after laser exposure. The famous Interleukin 10, anti inflammatory protein doubled the levels, endorfines were released in high levels.
It has been established that the photobiomodulation process will give extraordinary benefits in pain management or inflammation, immunomodulation, and promotion of wound healing and tissue regeneration, and it plays a fundamental part in our protocols.
Isn’t it all short of amazing?
Will see you in the next blog. Keep your cells healthy!
- Published in Corporate News / Blog
PRP and Stem Cell Treatments Being Studied for Hair Loss
Hair loss is very common, with tens of millions, if not hundreds of millions of people all over the world suffering from it. Hundreds of thousands of people decide to utilize hair restoration therapy, as well as other procedures in order to try to get at least some of their former hair back. Although some are effective, most of the time, the treatments only move already existing hair from one place to another. However, with Stem Cell therapy, we try to help new hair grow by helping the follicles to regenerate.
Adimarket helps, alongside a few other companies, to help provide new and reliable uses for PRP and stem cell therapies. We provide the equipment and other services so that doctors and practices will be able to provide these services to their patients.
There’s a Lot of Promise
While the main people talking about PRP and stem cell therapies are smaller companies like us, many other people are also discussing and seeing potential in these therapies. These include doctors, and practices, such as a doctor from Miami known as Lazaro M Garcia Md. This doctor already utilized PRP and stem cell therapy for people who suffer from hair loss, and is currently conducting a study that is supported by the National Institutes of Health.
In order to participate in the study, patients pay a small fee, which changes based on what part of the study they are in. Afterwards, the receive 2 injections of PRP and stem cells that are made from their own body, over 3 months.
Dr. Garcia is utilizing the body’s own growth factors in order to increase the amount of blood and nutrients to the otherwise dead hair follicles. This makes the dead follicles more lively and allows them to create new hair growth.
The way to make Platelet Rich Plasma is to is to use the patients own blood, which can come from either bone marrow, or other sources of fat. They go into a centrifuge, which concentrates the composition, and then allows them to be injected into the treatment site. While it is an otherwise simple procedure, some training in still necessary to ensure that it is done safely.
We Provide Equipment
We at Adimarket do not perform stem cell and PRP therapies, but we do offer the equipment so that doctors and practices can do so themselves. These include amniotic tissue, stem cell and PRP kits, centrifuge devices, and many more. Practices and doctors can order directly from us.
It is good to note that not all PRP systems are equal. The system that we have uses the closed tabletop system that is able to process the PRP in under 10 minutes. For more information, contact us or visit our website.
Hair loss is a serious problem with many people suffering from it. Now, thanks for PRP and stem cell therapies, we no longer only have to rely on hair replacement surgery to help patients. PRP and stem cell therapies may be the best therapy out there for both your patients, as well as your practice.
- Published in Corporate News / Blog
Top 3 Reasons we offer doctors marketing services
Here at Adimarket, we sell equipment to practices that are willing and able to add PRP and stem cell therapies to their lineup. The equipment we offer is among the best, and we have helped hundreds of doctors and practices to offer PRP and stem cell therapies. However, we also provide marketing services above that as well.
Although it might see odd that we offer both marketing services, as well as equipment, but it is not so odd once you understand why. Simply offering services and having the equipment to do so does not in itself help patients to fully know that you are offering new services. It is best practice to get the word out to as many people in the area as possible.
While there are many reasons why we do this, here are the three main reasons why.
Regenerative Medicine Was Founded Not Too Long Ago
Compared to many other medical practices, such as surgery and physical therapy, regenerative medicine is still fairly new. In fact, most people do not really know that PRP and stem cell therapy even exists, let alone can be used to manage chronic pain.
The fact that not many people even know about the existence of regenerative medicine, let alone what it can be used for, means that it would be difficult to get your patients to even understand what you are offering as a service. This can be addressed with marketing. Through marketing, a practice can not only let it become known that they are offering these new services, but also explain shortly what the service entails.
Marketing Is Like Dieting
Pretty much every doctor and dietitian knows that good nutrition is vital to great health down the line. Waiting until you’re sick and deficient to discuss nutrition is not the best way to address the issue. Marketing is similar in that instance. Marketing not only can be used to keep current patients informed, but can also be used to inform new patients about what you offer. Practices that don’t market often suffer in the same way as people who don’t get good nutrition.
There’s a lot of competition
Medicine has sadly become more and more like a business in the past years. This means that even doctors and practices need to have a good business sense if they are going to continue to be able to provide the type of services that patients need and desire. Not understanding business would only make any practice fail or at least prevent them from growing.
Because of this, private practices, as well as other medical groups are forced to compete. Marketing is a big way to make sure that you get patients instead of your competition. If you are utilizing PRP and stem cell therapies as a way to generate more income, then great! However, you will still have to market those services to get the word out, as well as compete.
We at Adimarket offer these services as a way to help the field of regenerative marketing succeed. We not only help your practice start to utilize regenerative medicine, but we also help you to promote your practice in the same way. This will help your patients know that you are using these methods, and what they are, so that you can get a leg up over the competition.
- Published in Corporate News / Blog
IFATS Recommendations for FDA Regulation of Human Cells, Tissues, and Cellular and Tissue-Based Products
International Federation of Adipose Therapeutics and Sciences (IFATS)
45 Lyme Road – Suite 304
Hanover, NH 03755 USA
Tel: 1-603-643-2325, Fax: 1-603-643-1444
September 26, 2016
Division of Dockets Management (HFA–305) Food and Drug Administration
5630 Fishers Lane, Rm. 1061
Rockville, MD 20852
Re: FDA-2014-D-1856 – Comments to 2014-2015 Draft Guidance regarding:
- Docket FDA-2014-D-1584: “Same Surgical Procedure Exception under 21 CFR 1271.15(b): Questions and Answers Regarding the Scope of the Exception; Draft Guidance for Industry”;
- Docket FDA-2014-D-1696: “Minimal Manipulation of Human Cells, Tissues, and Cellular and Tissue-Based Products; Draft Guidance for Industry and Food and Drug Administration Staff”;
- Docket FDA-2014-D-1856: “Human Cells, Tissues, and Cellular and Tissue-Based Products from Adipose Tissue: Regulatory Considerations; Draft Guidance for Industry”;
- Docket FDA-2015-D-3581: “Homologous Use of Human Cells, Tissues, and Cellular and Tissue- Based Products; Draft Guidance for Industry and FDA Staff.”
Dear Sirs and Madams:
The International Federation of Adipose Therapeutics and Sciences (IFATS) appreciates this opportunity to submit the following comments to supplement its earlier written comments and recent testimony at the September 12-13, 2016 Public Hearing on the 2014-2015 Draft HCT/P Guidances concerning: a) Minimal Manipulation; b) Same Surgical Procedure; c) Adipose Tissue; and d) Homologous Use.
IFATS is committed to the responsible advance of the science and translation of new adipose therapies, and it is determined to ensure patient safety. It was founded in 2003 by pioneering adipose stem cell biologists and clinician–scientists with the goal of advancing the science of adipose tissue biology and its clinical translation to therapeutic applications. Since that time, IFATS has remained at the forefront of regenerative medical applications involving adipose tissue and cells. Membership now spans 40 countries in North America, Europe, Africa, the Middle East, Asia, Australia, and Central and South America, and includes basic scientists, translational researchers, clinicians, and regulatory and biotech representatives. IFATS is formally aligned with, and its members serve on the editorial boards of the prestigious journals, Stem Cells and Stem Cells Translational Medicine. With the International Society for Cellular Therapy (ISCT), IFATS has provided the scientific community with a detailed description and definition of adipose derived cells (both stromal vascular fraction, or SVF, and adipose-derived stromal/stem cells, or ASCs) in the formal publication entitled Cytotherapy. Thus, IFATS possesses the necessary expertise to assist regulatory agencies in understanding adipose tissue, and regulating the safety and efficacy of adipose-related products and therapies.
Drawing on this expertise, IFATS has reviewed the 4 draft guidances with great care. It respectfully requests the FDA to reconsider and modify the 4 draft HCT/P guidances as follows:
Recommendation #1 – Cell-Based Risks: Interpret and evaluate an HCT/P’s homologous use and minimal manipulation based on its manufacturer’s intended use in the patient.
Recommendation #2 – Provider-Based Risks: Reduce provider-created risks by targeting provider behavior.
Recommendation #3: Recognize that adipose HCT/Ps have both structural and nonstructural functions, and regulate based on its manufacturer’s intended use in the patient.
Recommendation #4: Revise the evaluation of minimal manipulation and homologous use as they pertain to particular applications of adipose tissue.
◊ ◊ ◊ ◊ ◊ ◊ ◊
IFATS recognizes the FDA’s challenge in developing regulations that fulfill the agency’s dual and interrelated responsibilities of protecting patients while promoting innovation. IFATS further recognizes that although these are complementary rather than competing objectives, they are often difficult to pursue simultaneously. The FDA’s 3-tiered, risk-based §§ 361 – 351 framework balances these concerns by making the degree of regulatory oversight proportionate to the degree of an HCT/P therapy’s risk.
The concepts of homologous use and minimal manipulation are key determinants of whether an HCT/P will be classified as a § 361 product (which does not need premarket approval) or a § 351 drug, device and/or biological product (which requires formal premarket approval). The applicability of § 351’s “same surgical procedure” exception also turns on homologous use and minimal manipulation. For most manufacturer-clinicians, § 351 categorization raises insurmountable obstacles due to the time and expense of obtaining premarket approval. In such cases, § 351 classification effectively prohibits access to safe and effective HCT/P therapies, even when those therapies involve a patient’s own cells and/or can deliver superior results with reduced risks. At the same time, § 351 oversight is essential for therapies that pose greater risks due the HCT/P’s characteristics, mechanism(s) of action and circumstances of use.
A second type of risk involves rogue clinicians offering false promise in the form of unproven therapies performed with few safeguards and less training. Provider misconduct is not unique to HCT/P therapies; it pervades all areas of medical practice. Nevertheless, IFATS shares the FDA’s alarm over such practices in the context of HCT/Ps, and is equally determined to curtail them. Because a solution cannot solve a problem without identifying and attacking its root cause, effective regulation of HCT/P-related risks must recognize and respond to their multivariate causes. Put simply:
- Sections 351 and 361 appropriately attempt to regulate HCT/P therapies proportionate to the risks of unpredictable and/or unsafe cell behavior.
- However, the risks of untrained providers misusing HCT/P therapies are caused by providers misbehaving, not cells misbehaving.
Consequently, interpretive guidance that restricts the definition and application of HCT/P terminology can only go so far in restricting provider-based risks. In addition, restrictive, inaccurate or imprecise definitions and interpretations carry their own risks of restricting access to therapies and restricting a patient’s right to evaluate risk through the process of informed consent.
Therefore, IFATS recommends that the FDA adopt an overall two-part strategy that focuses on both categories of HCT/P risks, i.e., those relating to cell behavior and those that pertain to provider behavior.
Recommendation #1 – Cell-Based Risks:
Interpret and evaluate an HCT/P’s homologous use and minimal manipulation based on its manufacturer’s intended use in the patient. Interpretive guidance should predicate each definition on to the functions and/or characteristics of the specific composition (i.e., cell type(s) and/or matrix or other component(s)) that are involved in, and/or relevant to the manufacturer- clinician’s intended use in the patient.
Recommendation #2 – Provider-Based Risks:
To reduce provider-created risks, the FDA should target provider behavior by collaborating with IFATS and comparable organizations to draw on and supplement existing federal and state methods of certification, registration, and similar measures.
Adopting this two-part strategy can control risk more comprehensively – and therefore more effectively – in furtherance of the FDA’s dual and interrelated obligations of protecting patients and promoting the availability of HCT/P therapies. IFATS explains each recommendation as follows:
Recommendation #1 – Cell-Based Risks: Interpret and evaluate an HCT/P’s homologous use and minimal manipulation based on its manufacturer’s intended use in the patient.
The four draft guidances on homologous use, minimal manipulation, same surgical procedure and adipose tissue individually and collectively intend to “improve stakeholders’ understanding” of 21 CFR 1271 by clarifying the FDA’s interpretation of homologous use and minimal manipulation. As demonstrated by the initial round of public comments and the ensuing public hearing on September 12 and 13, 2016, the draft guidance documents have not clarified applicable regulations. They have instead compounded the difficulty of understanding and complying with them. The drafts’ introduction of new definitional inaccuracies has also amplified rather than reduce patient risk.
IFATS respectfully requests the agency to clarify the definitions and application of homologous use and minimal manipulation by interpreting each as referring to the characteristics of the specific cell type(s) and/or the matrix or other component(s) that are involved in, and/or relevant to the manufacturer’s intended use in the patient. Thus, the definition of homologous use with interpretive guidance would read as follows:
21 CFR 1271.3(c): Homologous use means the repair, reconstruction, replacement, or supplementation of a recipient’s cells or tissues with an HCT/P that performs the same basic function or functions in the recipient as in the donor.
Recommended GUIDANCE: As used in this section, “performs the same basic function or functions in the recipient as in the donor” shall be interpreted as referring to one or more of the function(s) of the specific composition of the therapeutic/product, reflecting the specific cell type(s) and/or the specific matrix or other component(s) in the donor tissue that are involved in, and/or relevant to the manufacturer’s intended use in the patient.
Similarly, the definition of minimal manipulation with interpretive guidance would read as follows:
21 CFR 1271.3(f) Minimal manipulation means:
- For structural tissue, processing that does not alter the original relevant characteristics of the tissue relating to the tissue’s utility for reconstruction, repair, or replacement;
- For cells or nonstructural tissues, processing that does not alter the relevant biological characteristics of cells or
Recommended GUIDANCE: As used in this section, “relevant” characteristics shall be interpreted to mean the characteristics of the specific cell type(s) and/or the specific matrix or other component(s) in the donor tissue that are involved in, and/or relevant to the manufacturer’s intended use in the patient.
Rationale: Incorporating and relying on the manufacturer’s intended use harmonizes the interpretation and definition of homologous use and minimal manipulation with statutory directives to predicate the regulation of drugs, devices and biologics on the manufacturer’s intended use.
Defining relevant characteristics in terms of “the characteristics of specific cell type(s) and/or the matrix or other component(s) in the donor tissue that are involved in, and/or relevant to the manufacturer’s intended use in the patient” promotes patient safety by insisting on a reasonable and scientifically supportable rationale for using an HCT/P for a particular mechanism of action. This clarification balances the FDA’s dual responsibilities of protecting patients from undue safety risks while promoting the ongoing availability and continued development of HCT/P therapies.
Example of Non-Homologous Use: Decellularized adipose matrix used to accomplish the manufacturer’s intended use of a particular metabolic or systemic effect in the patient (e.g., reducing insulin levels in a diabetic patient) is non-homologous because decellularized matrix is not relevant to metabolic or systemic activity.
◊ ◊ ◊ ◊ ◊ ◊ ◊
Recommendation #2 – Provider-Based Risks: To reduce provider-created risks, the FDA should target provider behavior by collaborating with IFATS and comparable organizations to draw on, and supplement existing federal and state methods of certification, registration, and similar measures.
For a risk-reduction strategy to succeed, it must target the root cause of the risk. Revising, retracting or replacing interpretations of regulatory terminology can target the risks of cells behaving in an unsafe ways, but can do little to prevent providers from behaving in unsafe ways. Because the risks of irresponsible providers offering unsafe treatments are not exclusive to HCT/P therapies, many federal and state mechanisms already exist for identifying, disciplining and prohibiting clinics and clinicians from endangering patients.
IFATS shares the FDA’s concern about provider-related risks in the HCT/P sector and shares its determination to end or minimize these risks. IFATS respectfully requests the FDA to collaborate with it and comparable organizations to identify and draw on existing federal and state methods for curtailing provider misconduct, and developing additional protections in the form of provider certification, registration, monitoring and similar measures. At present, the §§ 351-361 regulatory framework does not – and cannot – adequately respond to this form of risk. Collaboration among stakeholders and coordination with existing means of provider oversight offers the most effective and efficient strategy for protecting patients from provider-created risk.
Therefore, IFATS respectfully requests the FDA to meet with IFATS, the American Association of Blood Banks and other accreditation bodies for the purpose of working together to identify provider-focused safety objectives and measures that can be translated into formal accreditation requirements and interpretive guidance.
◊ ◊ ◊ ◊ ◊ ◊ ◊
Recommendation #3: Recognize that adipose HCT/Ps have both structural and nonstructural functions, and regulate based on its manufacturer’s intended use in the patient.
IFATS requests the FDA to expand its definition of adipose tissue from exclusively structural in function to include both structural and/or nonstructural functions, depending on the manufacturer’s intended use in the patient. This modification is critically necessary in order to:
- Reconcile the interpretive guidance on the definition and regulation of adipose with applicable statutory and regulatory requirements;
- Reflect and ensure biological accuracy; and most importantly,
- Regulate an HCT/P’s risks based on the manufacturer’s intended use and mechanisms of action in the patient.
More specifically:
a. Recognizing adipose tissue’s structural and/or nonstructural functions is required by applicable statutory and regulatory requirements.
Adipose HCT/Ps must be defined as having structural and/or nonstructural functions to align the draft guidance with statutory and regulatory recognition that cells and tissues may have more than one function. According to 42 USC § 321(g)(1), “[t]he term ‘drug’ means … (B) articles intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease in man or other animals; and (C) articles (other than food) intended to affect the structure or any function of the body of man or other animals; and (D) articles intended for use as a component of any article specified in clause (A), (B), or (C). (emphasis added). Statutory directives to focus on intended use pervade FDA regulation, including the regulation of drugs, biologics, devices, cosmetics, pesticides and more. Applicable statutes and regulations explicitly and implicitly recognize that the human body is complex, and its tissues and cells are often versatile and multi-functional. For example, 21 CFR 1271.3(c)’s definition of homologous use correctly recognizes that an HCT/P may have more than one “basic function.” It never says or even suggests that an HCT/P can only have one function, or that the regulator has sole authority to define that function and thereby dictate a manufacturer’s intended use. And yet the draft guidances do just that by insisting that adipose HCT/Ps are solely structural.
To align interpretive guidance with the regulations and statutory provisions being interpreted, IFATS respectfully requests the FDA to avoid pre-determining specific functions and uses for specific HCT/Ps. Instead, it should base regulations and guidance on the HCT/P’s function(s) and characteristic(s) that are relevant to its intended use by the manufacturer.
b. Recognizing adipose tissue’s structural and/or nonstructural functions is necessary to correct factual inaccuracy.
Regulation 21 CFR 1271.10(a)(4) categorizes an HCT/P as “either” structural or nonstructural, depending on its function. A structural HCT/P “does not have a systemic effect and is not dependent upon the metabolic activity of living cells for its primary function.” A nonstructural HCT/P “has a systemic effect or is dependent upon the metabolic activity of living cells for its primary function.”
The draft adipose guidance expressly acknowledges that adipose tissue contains adipocytes, preadipocytes, fibroblasts, vascular endothelial cells, a variety of immune cells, and also stores energy in the form of lipids. Citing only Junqueira ’s Basic Histology: Text & Atlas , the draft guidance classifies adipose as a connective and therefore structural tissue. This result is internally inconsistent and factually inaccurate – and the FDA’s sole cited authority explains why.
Junqueira classifies connective tissue as: 1) connective tissue proper; 2) embryonic connective tissues; and 3) specialized connective tissues. The latter category defines specialized connective based on their principal specialized functions. Blood, reticular connective tissue, adipose tissue, bone and cartilage all qualify as specialized connective tissues with specialized, nonstructural functions. Junqueira ’s examples include the following:
- Blood is a specialized connective tissue; its principal function of transport is nonstructural.
- Reticular connective tissues include the liver, pancreas, bone marrow and lymph They are nonstructural tissues because their principal functions are metabolic, including endocrine.
- According to Junqueira – the FDA’s sole cited authority – adipose tissue is nonstructural specialized connective tissue; its primary function is metabolic with co-existing structural
Junqueira ’s categorization of adipose as primarily nonstructural reflects longstanding scientific consensus. In1893, Gustav Neuber described his use of fat grafting in the orbital region to heal the adherent scarring which was the sequela of osteomyelitis. As a result of its nonstructural healing functions, the fat graft transformed facial scarring to more normal appearing skin and subcutaneous tissues. [6] In 1912, Holländer described the successful use of fat injections to prevent the recurrence of scarring following breast surgery. [7] In 1926, Charles Conrad Miller developed a new system for injecting fat grafts, and described 36 cases of correcting cicatricial contraction on the face and neck, and reported “excellent results” for another 2 cases after using fat grafts to treat “very persistent parotid fistulas…which defied all other methods of treatment.” [8] These and similarly favorable outcomes resulted from fat’s transformational nonstructural repair of the tissues into which it was placed. [8]
The understanding of the diverse roles of adipose tissue has steadily expanded [9], due in large part to the discovery of the first widely accepted adipokine, leptin, in the mid-1990’s. [10] Adipose tissue secretes proteins with systemic actions on hematopoietic, reproductive, metabolic, and other cells and tissues demonstrates unequivocally that adipose meets the definition of a true “endocrine” organ.[11,12] A Google scholar search of all available online medical and research databases for “the primary function of Adipose Tissue” returns 538,000 journal articles. Although the search did not designate a specific function, the search results referred to adipose tissue almost exclusively as a nonstructural metabolic and endocrine organ with secretory properties. A search for an exact match of the phrase “primary function of adipose tissue” yielded the following: “It was long believed the primary function of adipose tissue was energy storage; in fact, stromal adipose is a complicated endocrine organ.” However, even energy storage is nonstructural.
The FDA’s draft guidance on minimal manipulation defines nonstructural tissues as “serv[ing] predominantly metabolic or other biochemical roles in the body such as hematopoietic, immune, and endocrine functions.” To illustrate, the draft guidance offers “cord blood, lymph nodes, pancreatic tissue” as examples of nonstructural tissue. These tissues are indeed nonstructural – but they are also specialized connective tissue, as explained in Junqueira. In addition adipose has “hematopoietic, immune, and endocrine functions,” as explained below. As demonstrated by Junqueira, adipose HCT/Ps clearly do more than “reconstruction, repair, or replacement that relate to its utility to cushion and support the other tissues in the subcutaneous layer (subcutaneum) and skin.” And the FDA’s own nonstructural examples prove that classifying connective tissue, including adipose tissue as solely structural is factually inaccurate and logically flawed.
Thus, IFATS strongly recommends that the draft guidances be revised to define and categorize adipose tissue has both structural and nonstructural functions.
In support, IFATS offers the following examples of adipose’s nonstructural, and combined nonstructural and structural functions.
Nonstructural Functions of Adipose HCT/Ps:
- Nonstructural Endocrine Functions – It is well recognized that adipose is an endocrine organ which, like other endocrine organs, performs a variety of nonstructural Adipose tissue secretes proteins with nonstructural, systemic actions on hematopoietic, reproductive, metabolic, and other cells and tissues. [11, 12]
Examples:
- Glucose and lipid metabolism control via adipokine secretion [13]
- Reproductive and endocrine control via adipokine secretion [14-16]
- Immunomodulatory and immunosuppressive systemic control via cytokine and protein factor secretion [17-22]
2. Nonstructural Paracrine Functions
- Angiogenic control via vasculogenic cytokine secretion [22-26]
- Hematopoietic control via cytokine secretion, both locally and systemically [27]
- Neurogenesis via secretion of cytokine factors [28-34]
3. Nonstructural Hematopietic Potential of adipose stem cells in adipose deposits
- Reservoir for hematopoietic and lymphoid progenitor cells similar to bone marrow [18, 35, 36]
- Thermogenesis (brown and beige fat)[37-41]
- Energy reservoir (white adipose depots) [42,43]
4. Nonstructural Promotion of Lactation
- Fat serves as an energy reservoir and nutrient supply for breast epithelial cells.
- As pregnancy progresses, the breast epithelium proliferates in a branching manner to occupy the majority of the adjacent adipose tissue and
- At parturition, the epithelial cells draw on the lipid reserves of adipocytes within immediate proximity and secrete these nutrients into the milk available to the newborn infant during
- As long as the mother continues to breast feed the infant, the epithelial cells remain viable and
- If suckling is discontinued for periods of 24 to 48 hours, the epithelial cells undergo rapid apoptosis, leaving pre-adipocytes and adipocytes as the predominant cell within the breast
- While the presence and organization of epithelial cells within the breast tissue provide it with a unique architecture, the mammary adipocytes themselves show remarkable similarity to adipocytes from elsewhere in the Thus, the mammary fat pad displays homology to other adipose tissue depots.[44]
5. Nonstructural Regenerative Functions
- Local and circulating multipotent progenitor cells can repair and regenerate damaged tissues such as repairing irradiated skin, alleviating fibrotic changes, improving mobility and vitality, and repairing structures such as hair follicles and [45-47]. Specific examples include:
- Modulation of scarring
- Treatingold burn scars [55-57]
- Release of adherent scarring/fasciotomies [58]
- Modulation of scarring in primary cleft lip repair [59]
- Multipotent progenitor cells may be recruited for repair and regeneration of ischemic damage induced by acute myocardial infarction. [48]
- Adipose mesenchymal stem cells as progenitor cells in a perivascular position contribute to vascular network formation and vascular structures.[49-52] As such, the adipose mesenchymal stem cells are located in a position and serve a role shared by mesenchymal stem cells located in nearly all body tissues [53]. Adipose MSCs located in a range of tissues can enhance vascularity and perfusion, and thus provide cells that are precisely homologous to those already present in the
- Adipose mesenchymal stem cells induce a monocyte/macrophage phenotype switch from M1 to M2 macrophages, contributing to improved infarct healing post-acute myocardial [54]
6. Nonstructural Functions in Bone Marrow – Bone marrow and blood products are exempt from regulation under § 351 and 361. For over 40 years, it has been clearly established that adipose is present in bone marrow where it serves a wide variety of nonstructural functions. The following physiologic processes have nothing to do with providing cushioning and support and therefore are not properly categorized as a structural use or function of adipose cells. [3]
- Pre-adipocytes as mesenchymal cells in bone marrow: Bone marrow contains a spectrum of mesenchymal cells, including pre-adipocytes that can perform the nonstructural function of differentiating into adipocytes, osteoblasts and chondrocytes depending on the organism’s current needs.
- Pre-adipocytes and adipocytes regulate lympho-hematopoiesis and enable the bone marrow microenvironment to regulate proliferation within blood cell lineages to favor erythropoiesis rather than Adipocytes also contain nonstructural metabolic precursors and energy for the purpose of lympho-hematopoiesis. This is a nonstructural function.
- Adipocytes are essential for synthesizing plasma membranes during blood cell development because they contain cholesterol esters, triglycerides and lipoproteins.
- Bone marrow and extramedullary adipocytes are critical for homeostatic control of temperature in the bone marrow microenvironment and throughout the body, and thus contribute to the overall energy metabolism of the organism.
- Bone marrow adipose tissue is an essential endocrine organ.[4] Bone marrow adipose tissue (MAT) increases during caloric restriction (CR), is responsible for increased adipokine secretion, and alters skeletal muscle adaptation to These and other observations identify MAT as an endocrine organ.
BOTH Nonstructural and Structural Functions: In the following examples, adipose’s structural and nonstructural functions combine for the patient’s benefit:
- Reversal of damage caused by therapeutic radiation [60-63]
- Structural (filling tissue defect) uses, and
- Nonstructural tissue repair and regenerative uses [63]
- Treatingacute thermal injury [64-65]
- Treating Pain Mitigating implant breast pain [66]
- Improving post-mastectomy pain [67-68]
- Improving lower back pain [70]
- Nerveor neuroma repair [71-72]
- Healing ulcers
- Treatingpressure sores [73]
- Treating chronic non-healing anal fissures and associated stenosis [74]
- Treating vocal fold paralysis [75-77]
- Treating velopharyngeal insufficiency [78]
- Treating scleroderma and systemic sclerosis [79]
- TreatingDupuytren’s disease of the hand [80, 81]
- Treating Raynaud’s phenomenon – After fat grafting, there is improved symptomatology with evidence suggestive of measurably increased perfusion [82]
- Improving tendon repair
- Adipose tissue assists in tenolysis for foot and hand tendon [83]
- Treating adherent tendons and joints in burn patients with fat graft [84]
- Preventing osseous reunion of skull defects [85]
- Improvingthe quality of skin [86]
c. Regulating an HCT/P’s risks based on the manufacturer’s intended use and mechanisms of action in the patient ensures meaningful evaluation and effective regulation of risk.
The §§ 351-361 framework conditions the degree of regulatory oversight on the degree of an HCT/P’s risk. The homologous use and minimal manipulation criteria are central to determining whether an HCT/P will be classified as a § 361 or § 351 product, and if the latter, whether § 351’s “same surgical procedure” exception will apply. In turn, the existence of homologous use and minimal manipulation depend on the HCT/P’s structural or nonstructural function. More specifically:
21 CFR 1271.3(c) defines homologous use as “the repair, reconstruction, replacement, or supplementation of a recipient’s cells or tissues with an HCT/P that performs the same basic function or functions in the recipient as in the donor.”
21 CFR 1271.3(f) evaluates minimal manipulation of structural tissue in terms of processing that does not alter “the original relevant characteristics of the tissue relating to” the tissue’s utility for reconstruction, repair, or replacement. For nonstructural tissues, it evaluates “the relevant biological characteristics of cells or tissues.”
Insisting that adipose be evaluated as exclusively structural precludes any evaluation of its nonstructural functions despite their presence and importance in the donor and intended use and therapeutic benefits for the recipient. Failing § 361’s homologous use and minimal manipulation criteria are virtually guaranteed. This effectively prohibits any nonstructural use, and precludes any meaningful evaluation of their risks.
As a result, it effectively prohibits patient access to safe nonstructural applications of adipose tissue and thereby undermines the FDA’s obligations to protect patients and promote innovation.
The “ same surgical procedure” exception to § 351 also becomes completely unavailable for nonstructural use of adipose because it similarly requires homologous use and minimal manipulation.
◊ ◊ ◊ ◊ ◊ ◊ ◊
Recommendation #4: Revise the evaluation of minimal manipulation and homologous use as they pertain to particular applications of adipose tissue, (as detailed below).
IFATS respectfully requests the FDA to reconsider three particular applications of adipose tissue with regard to homologous use and minimal manipulation, each of which is required for § 361 classification as well as § 351’s “same surgical procedure” exception. In specific, IFATS requests the FDA to change its prior examples of the absence of homologous use and/or minimal manipulation to recognize the following:
- Decellularizing adipose tissue for structural use is minimal manipulation.
- Structural use of fat in the breast constitutes homologous
- Stromal vascular fractionation (SVF) of adipose to obtain nonstructural adipose components for use as a nonstructural tissue constitutes minimal
Each is explained in order
a. Decellularizing adipose tissue for structural use is minimal manipulation.
The draft guidance currently states that decellularizing structural adipose tissue constitutes more than minimal manipulation because the process alters the tissue’s ability to perform structural functions. This is incorrect. Adipose tissue’s structural functions are performed by a dense and interconnected skeleton of reticular fiber and dense connective tissue. Its biomechanical properties include tensile strength and elasticity, both of which are central to the structural functions of padding and cushioning.
Nonstructural components such as adipocytes, pre-adipocytes, lipids, etc. do not contribute to adipose’s structural characteristics or functions. It is well recognized that decellularization leaves adipose’s structural components fully intact. It does not alter, disturb or weaken the remaining reticular fiber and dense connective tissue skeleton, or compromise its ability to perform structural functions. Multiple reports have demonstrated that decellularized adipose tissue retains structural properties and can be injected to impart padding and cushioning of soft tissues. [89-93]
The FDA already classifies decellularized dermis as minimally manipulated, thereby acknowledging that the process of decellularization does not alter structural characteristics or functions of the remaining structural matrix. Removing cells from dermis and removing cells from adipose employ comparable methods to achieve comparable results. Decellularizing adipose for structural use, like decellularizing dermis for structural use, does not alter structural characteristics.
For these reasons, IFATS respectfully requests the FDA to revise the draft guidance to recognize that decellularized adipose is minimally manipulated as required by § 361 and § 351’s “same surgical procedure exception.”
b. Structural use of fat in the breast constitutes homologous use.
Example B-3 of the draft adipose guidance states that application of adipose-based HCT/Ps to the breast is nonhomologous use because “[t]he basic function of breast tissue is to produce milk (lactation) after childbirth. Because this is not a basic function of adipose tissue, using HCT/Ps from adipose tissues for breast augmentation would generally be considered a non-homologous use.” This logic is flawed and must be corrected because it mischaracterizes the function of the breast, and mischaracterizes the function of adipose in breast surgery.
- For the purpose of determining homologous use, the basic function of the breast is a secondary sex organ. In terms of shape, form and appearance, the breast is vital to a woman’s bodily integrity and body image, psychological sense of self, and overall physical and emotional health and well-being.
- Lactation is not the sole or even primary function of the breast.
- Most women never lactate, but their breasts do function as secondary sex organs throughout their adolescence and
- When lactation does occur, it is episodic, time-limited, and accounts for a very small fraction of a woman’s lifespan.
- Even when healthy, post-menopausal women cannot Restoring lactation is thus completely irrelevant to restoring breast function.
- All men have breasts, thousands develop breast cancer each year, and many will need reconstructive surgery — even though men do not lactate.
- Federal law recognizes and protects the breast’s importance as a secondary organ.
- The Women’s Health and Cancer Rights Act, 29 USC 1185b(a), requires group health insurers to cover “all stages” of breast reconstruction following mastectomy or irradiation, including bilateral correction of asymmetrical appearance where one breast is otherwise unaffected.
- Restoring lactation is not a goal or even a remote concern of this In fact, lactation is never mentioned in the statute’s text, legislative history or associated regulations.
- The function of adipose tissue in breast surgery is structural and therefore
- Mastectomy removes more than the ability to lactate. It removes size, shape and form by removing the breast mound, which is predominantly adipose. Consequently, applying adipose tissue for the structural purpose of restoring form and shape is homologous use.
- By classifying adipose based tissues as non-homologous when applied to the breast, an entire class of Centers for Medicare & Medicaid Services (CMS) approved breast reconstruction procedures would be at risk for not complying with the same surgical procedure For example:
- Autologous free tissue flap transfer (“free flap” breast reconstruction) is performed by transferring complex musculocutaneous flaps containing adipose One of the most common methods of reconstruction, it qualifies as an HCT/P because it completely removes fat-containing tissue flaps from the body before implanting. [94-96] Fat grafting for breast reconstruction is another common clinical practice.
- According to the draft adipose guidance, these and other methods of breast reconstruction could no longer be used without formal premarket approval because they do not restore lactation and are therefore non-homologous. Focusing solely on restoration of lactation ignores the fact that the breast is largely composed of fat tissue and its size, shape and form can be reconstructed with fat
- This and other methods of breast reconstruction will no longer be available for clinical use under 361 or § 351’s same surgical procedure exception because they will not restore lactation.
- Removing these and other reconstructive methods from clinical application has nothing to do with risk. It is instead a perverse outcome of insisting that breast reconstruction be evaluated for its ability to restore the breast’s minor and episodic function of lactation despite fat’s ability to restore the breast’s size, shape and function as a secondary sex organ.
For these reasons, IFATS respectfully requests the FDA to revise the draft HCT/P guidance documents to recognize that as applied to the breast, adipose tissue is homologous use because it performs the structural functions of restoring, repairing or reforming size, form and shape.
c. When intended for a nonstructural use in the patient, stromal vascular fractio n (SVF)cells should be evaluated as nonstructural when determining minimal manipulated and homologous use.
The FDA’s draft adipose guidance expressly acknowledges that adipose tissue contains a variety of nonstructural components, including adipocytes, preadipocytes, fibroblasts, vascular endothelial cells, a variety of immune cells, and also stores energy in the form of lipids. These are nonstructural because the cells perform the same regenerative functions in vivo as they do in vitro and animal models. [97- 98] Nonstructural adipose HCT/Ps are readily available in the stromal vascular fraction (SVF). Stromal vascular fractionation of lipoaspirate (typically obtained through liposuction) can remove fat’s structural components, making nonstructural SVF cells available for nonstructural use in a patient. Just as removing nonstructural cells through decellularization does not alter the relevant structural characteristics or structural function of the remaining structural matrix, removing structural components does not alter the relevant nonstructural characteristics or nonstructural function of the remaining nonstructural SVF components.
This is minimal manipulation under 21 CFR 1271.3(f)(2) because extracting nonstructural cells or tissues from lipoaspirate “does not alter the relevant biological characteristics of cells or tissues.”
Also, this is homologous use under 21 CFR 1271.3(c) because it uses lipoaspirate’s nonstructural HCT/Ps for “repair, reconstruction, replacement, or supplementation of a recipient’s cells or tissues with an HCT/P that performs the same basic function or functions in the recipient as in the donor.”
Examples: Nonstructural adipose tissue for homologous use, with minimal and more than minimal manipulation à Reversal of radiation damage as intended nonstructural use
Homologous use with no manipulation: Using liposuction aspirate to perform fat grafting/adipose tissue therapy for the intended use or of reversing radiation damage in the breast – a nonstructural function – is homologous use. The structural side-effect of increasing volume may be a collateral benefit, but the intended use is still nonstructural tissue repair.
- Use is homologous because the HCT/P performs that same basic nonstructural function in both donor and
Homologous use with minimal manipulation: Using liposuction aspirate is indicated for the nonstructural function of reversing radiation damage in the neck without the volume gain of a fat graft. Separating nonstructural from structural components obtains nonstructural SVF cells for nonstructural use in the patient.
- Use is homologous because it is performing the intended nonstructural function of reversing radiation
- Manipulation is minimal because processing does not alter relevant nonstructural biological characteristics.
Homologous use with more than minimal manipulation: Using liposuction aspirate is indicated for the nonstructural function of reversing radiation damage in the intestines by catheter injection of nonstructural SVF. However, an adequate dose is difficult to obtain because the patient is cachectic (low body fat caused by caloric depletion from radiation enteritis). Culture expansion is considered as a means of increasing dose.
- Use is again homologous because SVF cells would perform the intended nonstructural function of reversing radiation
- Manipulation is more than minimal because culture expansion of cells to yield a therapeutic dose alters relevant biological characteristic. SVF cells in their natural state do not engage in linear growth to create a homogeneous monoculture. Even tumors do not produce homogeneous monocultures.
Examples: SVF for nonhomologous use >>>Bone (re)generation
SVF cells do not normally form bone in their native location. Delivering SVF cells to bone for the intended structural function of directly (re)generating new bone (via action of “stem cells”) might be considered. Processing might involve combining SVF cells with one or more additives (such as ex vivo culture media additives) for the intended structural function of (re)generating NEW bone (such as additives added to our culture medias ex vivo). For this scenario:
- Use is nonhomologous because the basic function in donor and patient will differ if nonstructural SVF cells are combined with one or more additives (such as ex vivo culture media additives) for the intended structural function of (re)generating NEW bone (such as additives added to our culture medias ex vivo).
- Manipulation is more than minimal because processing would alter the nonstructural SVF’s original relevant characteristics.
◊ ◊ ◊ ◊ ◊ ◊ ◊
The members of IFATS are grateful for the FDA’s willingness to re-open and extend the period for public comments and allow additional time for the September 2016 public hearing on the 2014-2015 draft HCT/P draft guidances. As a multidisciplinary scientific society composed of adipose stem cell biologists and clinician–scientists, IFATS would greatly appreciate the opportunity to work with the FDA in meeting the challenges of regulating HCT/P therapies. We respectfully request that representatives of the FDA, including the Director of CBER, meet with members of IFATS to discuss the issues addressed herein as well as others that pertain to the advancement and regulation of adipose-based therapies.
Respectfully submitted on behalf of IFATS,
Adam J. Katz, MD, FACS
Chair, IFATS Regulatory Affairs Committee & IFATS Co-Founder University of Florida College of Medicine
Professor
Director of Plastic Surgery Research,
Laboratory of BioInnovation and Translational Therapeutics Division of Plastic Surgery, Department of Surgery
IFATS BOARD OF DIRECTORS
Bruce Bunnell, PhD
Tulane University / United States
Louis Casteilla, PhD
University of Toulouse / France
Sydney Coleman, MD
New York & Pittsburgh Universities / United States
Julie Fradette, PhD
Lavalle University / Canada
William Futrell, MD
Founders’ Board University of Pittsburgh / United States
Marco Helder, PhD
VU University Medical Center Amsterdam / The Netherlands
Adam J. Katz, MD, FACS
Founders’ Board University of Florida / United States
Ramon Llull, MD, PhD –
Founders’ Board University of Barcelona / Spain
Kacey Marra, PhD
University of Pittsburgh / United States
Ricardo Rodriguez, MD –
President (2016) Private Practice / Johns Hopkins / United States
Peter Rubin, MD, FACS – Chair, Founders’ Board Chairman of the Board
University of Pittsburgh / United States
Stuart K. Williams, PhD
University of Louisville / United States
MEMBERS–AT-LARGE
Jeff Gimble, MD, PhD
Pennington Biomedical / United States
Keith March, MD, PhD
Indiana University / United States
REFERENCES
- Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ, March KL, Redl H, Rubin JP, Yoshimura K, Gimble Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: A joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy. 2013;15:641-648
- Diaz-Flores L, Gutierrez R, Madrid JF, Varela H, Valladares F, Acosta E, Martin-Vasallo P, Diaz-Flores L, Pericytes. Morphofunction, interactions and pathology in a quiescent and activated mesenchymal cell niche. Histol Histopathol. 2009;24:909-969
- Gimble The function of adipocytes in the bone marrow stroma. The New Biologist. 1990;2:304-312
- Cawthorn WP, Scheller EL, Learman BS, Parlee SD, Simon BR, Mori H, Ning X, Bree AJ, Schell B, Broome Bone marrow adipose tissue is an endocrine organ that contributes to increased circulating adiponectin during caloric restriction. Cell metabolism. 2014;20:368-375
- Meunier P, Aaron J, Edouard C, VlGNON Osteoporosis and the replacement of cell populations of the marrow by adipose tissue: A quantitative study of 84 iliac bone biopsies. Clinical orthopaedics and related research. 1971;80:147-154
- N. Über die wiederanheilung vollstädig vom körper getrennter, die ganze fettschicht en- thaltender hautstucke. Zbl f Chir 1893;30:16-17
- Hollander E, Joseph Cosmetic surgery. Handbuch der Kosmetik. Leipzig, Germany: Veriag von Velt. 1912;688
- Miller Cannula implants and review of implantation technics in esthetic surgery: In two parts. Oak Press; 1926.
- Gimble JM Fat circadian biology. Journal of applied physiology. 2009;107:1629-1637
- Tartaglia LA, Dembski M, Weng X, Deng N, Culpepper J, Devos R, Richards GJ, Campfield LA, Clark FT, Deeds Identification and expression cloning of a leptin receptor, ob-r. Cell. 1995;83:1263-1271
- Salgado AJ, Gimble Secretome of mesenchymal stem/stromal cells in regenerative medicine.
Biochimie. 2013;95:2195
- Salgado AJ, Reis RL, Sousa N, Gimble Adipose tissue derived stem cells secretome: Soluble factors and their roles in regenerative medicine. Curr Stem Cell Res Ther. 2009
- Khan M, Joseph Adipose tissue and adipokines: The association with and application of adipokines in obesity. Scientifica. 2014;2014
- Vicennati V, Garelli S, Rinaldi E, Di Dalmazi G, Pagotto U, Pasquali Cross-talk between
adipose tissue and the hpa axis in obesity and overt hypercortisolemic states. Hormone molecular biology and clinical investigation. 2014;17:63-77
- Kargi AY, Iacobellis Adipose tissue and adrenal glands: Novel pathophysiological mechanisms and clinical applications. International journal of endocrinology. 2014;2014
- Maïmoun L, Georgopoulos NA, Sultan Endocrine disorders in adolescent and young female athletes: Impact on growth, menstrual cycles, and bone mass acquisition. The Journal of Clinical Endocrinology
& Metabolism. 2014;99:4037-4050
- McIntosh K, Zvonic S, Garrett S, Mitchell JB, Floyd ZE, Hammill L, Kloster A, Di Halvorsen Y, Ting JP,
Storms RW. The immunogenicity of human adipose‐derived cells: Temporal changes in vitro. Stem cells. 2006;24:1246-1253
- McIntosh KR, Frazier T, Rowan BG, Gimble Evolution and future prospects of adipose- derived immunomodulatory cell therapeutics. Expert review of clinical immunology. 2013;9:175-184
- McIntosh KR, Lopez MJ, Borneman JN, Spencer ND, Anderson PA, Gimble Immunogenicity of allogeneic adipose-derived stem cells in a rat spinal fusion model. Tissue Engineering Part A. 2009;15:2677-2686
- Mitchell JB, McIntosh K, Zvonic S, Garrett S, Floyd ZE, Kloster A, Di Halvorsen Y, Storms RW, Goh B, Kilroy G. Immunophenotype of human adipose‐derived cells: Temporal changes in stromal‐associated and stem cell–associated markers. Stem cells. 2006;24:376-385
- Gimble JM, Dorheim MA, Cheng Q, Medina K, Wang CS, Jones R, Koren E, Pietrangeli C, Kincade Adipogenesis in a murine bone marrow stromal cell line capable of supporting b lineage lymphocyte growth and proliferation: Biochemical and molecular characterization. European journal of immunology. 1990;20:379-387
- Frazier TP, McLachlan JB, Gimble JM, Tucker HA, Rowan Human adipose-derived stromal/stem cells induce functional cd4+ cd25+ foxp3+ cd127− regulatory t cells under low oxygen culture conditions. Stem cells and development. 2014;23:968-977
- Frazier TP, Gimble JM, Kheterpal I, Rowan Impact of low oxygen on the secretome of human adipose- derived stromal/stem cell primary cultures. Biochimie. 2013;95:2286-2296
- Miranville A, Heeschen C, Sengenes C, Curat C, Busse R, Bouloumie Improvement of postnatal neovascularization by human adipose tissue-derived stem cells. Circulation. 2004;110:349-355
- Rehman J, Traktuev D, Li J, Merfeld-Clauss S, Temm-Grove CJ, Bovenkerk JE, Pell CL, Johnstone BH, Considine RV, March Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation. 2004;109:1292-1298
- Planat-Benard V, Silvestre J-S, Cousin B, André M, Nibbelink M, Tamarat R, Clergue M, Manneville C, Saillan-Barreau C, Duriez Plasticity of human adipose lineage cells toward endothelial cells physiological and therapeutic perspectives. Circulation. 2004;109:656-663
- Kilroy GE, Foster SJ, Wu X, Ruiz J, Sherwood S, Heifetz A, Ludlow JW, Stricker DM, Potiny S, Green P, Halvorsen YD, Cheatham B, Storms RW, Gimble Cytokine profile of human adipose-derived stem cells: Expression of angiogenic, hematopoietic, and pro- inflammatory factors. J Cell Physiol. 2007;212:702-709
- Ribeiro CA, Fraga JS, Grãos M, Neves NM, Reis RL, Gimble JM, Sousa N, Salgado The secretome of stem cells isolated from the adipose tissue and wharton jelly acts differently on central nervous system derived cell populations. Stem Cell Res Ther. 2012;3:18
- Silva NA, Gimble JM, Sousa N, Reis RL, Salgado Combining adult stem cells and olfactory ensheathing cells: The secretome effect. Stem cells and development. 2013;22:1232-1240
- Cho YJ, Song HS, Bhang S, Lee S, Kang BG, Lee JC, An J, Cha CI, Nam DH, Kim. Therapeutic effects of human adipose stem cell‐conditioned medium on stroke. Journal of neuroscience research. 2012;90:1794-1802
- Egashira Y, Sugitani S, Suzuki Y, Mishiro K, Tsuruma K, Shimazawa M, Yoshimura S, Iwama T, Hara The conditioned medium of murine and human adipose-derived stem cells exerts neuroprotective effects against experimental stroke model. Brain research. 2012;1461:87-95
- Wei X, Du Z, Zhao L, Feng D, Wei G, He Y, Tan J, Lee WH, Hampel H, Dodel Ifats collection:The conditioned media of adipose stromal cells protect against hypoxia‐ischemia‐induced brain damage in neonatal rats. Stem Cells. 2009;27:478-488
- Wei X, Zhao L, Zhong J, Gu H, Feng D, Johnstone B, March K, Farlow M, Du Adipose stromal cells-secreted neuroprotective media against neuronal apoptosis. Neuroscience letters. 2009;462:76-79
- Zhao L, Wei X, Ma Z, Feng D, Tu P, Johnstone B, March K, Du Adipose stromal cells- conditional medium protected glutamate-induced cgns neuronal death by bdnf. Neuroscience letters. 2009;452:238-240
- Cousin B, André M, Arnaud E, Pénicaud L, Casteilla Reconstitution of lethally irradiated mice by cells isolated from adipose tissue. Biochemical and biophysical research communications. 2003;301:1016-1022
- Han J, Koh YJ, Moon HR, Ryoo HG, Cho CH, Kim I, Koh Adipose tissue is an extramedullary reservoir for functional hematopoietic stem and progenitor cells. Blood.2009
- Harms M, Seale Brown and beige fat: Development, function and therapeutic potential. Nature medicine. 2013;19:1252-1263
- Rahman S, Lu Y, Czernik PJ, Rosen CJ, Enerback S, Lecka-Czernik Inducible brown adipose tissue, or beige fat, is anabolic for the skeleton. Endocrinology. 2013;154:2687-2701
- Wu J, Cohen P, Spiegelman Adaptive thermogenesis in adipocytes: Is beige the new brown? Genes & development. 2013;27:234-250
- Krings A, Rahman S, Huang S, Lu Y, Czernik P, Lecka-Czernik Bone marrow fat has brown adipose tissue characteristics, which are attenuated with aging and diabetes. Bone. 2012;50:546-552
- van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, Drossaerts JM, Kemerink GJ, Bouvy ND, Schrauwen P, Teule Cold-activated brown adipose tissue in healthy men. N Engl J Med. 2009;360:1500-1508
- Peirce V, Carobbio S, Vidal-Puig The different shades of fat. Nature. 2014;510:76-83
- Enerbäck S, Gimble Lipoprotein lipase gene expression: Physiological regulators at the transcriptional and post-transcriptional level. Biochimica et Biophysica Acta (BBA)- Lipids and Lipid Metabolism. 1993;1169:107-125
- Rudolph MC, Neville MC, Anderson Lipid synthesis in lactation: Diet and the fatty acid switch. Journal of mammary gland biology and neoplasia. 2007;12:269-281
- Gimble JM, Katz AJ, Bunnell Adipose-derived stem cells for regenerative medicine. Circ Res. 2007;100:1249-1260
- Bellows CF, Zhang Y, Chen J, Frazier ML, Kolonin Circulation of progenitor cells in obese and lean colorectal cancer patients. Cancer Epidemiology Biomarkers & Prevention. 2011;20:2461- 2468
- Bellows CF, Zhang Y, Simmons PJ, Khalsa AS, Kolonin Influence of bmi on level of circulating progenitor cells. Obesity. 2011;19:1722-1726
- Krijnen PA NB, Meinster E, Vo K, Musters RJ, Kamp O, Niessen HW,, Juffermans LJ. Acute myocardial infarction does not affect functional characteristics of adipose derived stem cells in rats, but reduces the number of stem cells in adipose tissue. IFATS Annual Meeting. 2014:100
- Traktuev DO, Merfeld-Clauss S, Li J, Kolonin M, Arap W, Pasqualini R, Johnstone BH,March KL. A population of multipotent cd34-positive adipose stromal cells share pericyte and mesenchymal surface markers, reside in a periendothelial location, and stabilize endothelial networks. Circulation research. 2008;102:77-85
- Traktuev DO, Prater DN, Merfeld-Clauss S, Sanjeevaiah AR, Saadatzadeh MR, Murphy M, Johnstone BH, Ingram DA, March Robust functional vascular network formation in vivo by cooperation of adipose progenitor and endothelial cells. Circulation research. 2009;104:1410-1420
- Merfeld-Clauss S, Gollahalli N, March KL, Traktuev Adipose tissue progenitor cells directly interact with endothelial cells to induce vascular network formation. Tissue Engineering Part A. 2010;16:2953-2966
- Merfeld-Clauss S, Lupov IP, Lu H, Feng D, Compton-Craig P, March KL, Traktuev. Adipose stromal cells differentiate along a smooth muscle lineage pathway upon endothelial cell contact via induction of activin a. Circulation research. 2014;115:800-809
- Crisan M, Yap S, Casteilla L, Chen C-W, Corselli M, Park TS, Andriolo G, Sun B, Zheng B, Zhang A perivascular origin for mesenchymal stem cells in multiple human organs. Cell stem cell. 2008;3:301-313
- Ter Horst E, Naaijkens B, Krijnen P, Van Der Laan A, Piek J, Niessen Induction of a monocyte/macrophage phenotype switch by mesenchymal stem cells might contribute to improved infarct healing postacute myocardial infarction. Minerva cardioangiologica. 2013;61:617-625
- Guisantes E, Fontdevila J, Rodríguez Autologous fat grafting for correction of unaesthetic scars. Annals of plastic surgery. 2012;69:550-554
- Klinger M, Caviggioli F, Klinger FM, Giannasi S, Bandi V, Banzatti B, Forcellini D, Maione L, Catania B, Vinci Autologous fat graft in scar treatment. Journal of Craniofacial Surgery. 2013;24:1610-1615
- Klinger M, Marazzi M, Vigo D, Torre Fat injection for cases of severe burn outcomes: A new perspective of scar remodeling and reduction. Aesthetic plastic surgery. 2008;32:465-469
- Khouri RK, Smit JM, Cardoso E, Pallua N, Lantieri L, Mathijssen IM, Khouri Jr RK, Rigotti Percutaneous aponeurotomy and lipofilling: A regenerative alternative to flap reconstruction? Plastic and reconstructive surgery. 2013;132:1280-1290
- Balkin DM, Samra S, Steinbacher Immediate fat grafting in primary cleft lip repair. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2014;67:1644-1650
- Rigotti G, Marchi A, Galie M, Baroni G, Benati D, Krampera M, Pasini A, Sbarbati. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: A healing process mediated by adipose-derived adult stem cells. Plastic and reconstructive surgery. 2007;119:1409-1422
- Villani F, Caviggioli F, Klinger F, Klinger Rehabilitation of irradiated head and neck tissues by autologous fat transplantation. Plastic and reconstructive surgery. 2009;124:2190-2191
- Chang CC, Thanik VD, Lerman OZ, Saadeh PB, Warren SM, Coleman SR, Hazen Treatment of radiation skin damage with coleman fat grafting. STEM CELLS. 2007;25:3280-3281
- Sultan SM, Stern CS, Allen Jr RJ, Thanik VD, Chang CC, Nguyen PD, Canizares O, Szpalski C, Saadeh PB, Warren Human fat grafting alleviates radiation skin damage in a murine model. Plastic and reconstructive surgery. 2011;128:363-372
- Loder S, Peterson JR, Agarwal S, Eboda O, Brownley C, DeLaRosa S, Ranganathan K, Cederna P, Wang SC, Levi Wound healing after thermal injury is improved by fat and adipose-derived stem cell isografts. Journal of Burn Care & Research. 2015;36:70-76
- Sultan SM, Barr JS, Butala P, Davidson EH, Weinstein AL, Knobel D, Saadeh PB, Warren SM, Coleman SR, Hazen Fat grafting accelerates revascularisation and decreases fibrosis following thermal injury. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2012;65:219-227
- Cuomo R, Zerini I, Botteri G, Barberi L, Nisi G, D’ANIELLO Postsurgical pain related to breast implant: Reduction with lipofilling procedure. In Vivo. 2014;28:993-996
- Maione L, Vinci V, Caviggioli F, Klinger F, Banzatti B, Catania B, Lisa A, Klinger Autologous fat graft in postmastectomy pain syndrome following breast conservative surgery and radiotherapy. Aesthetic plastic surgery. 2014;38:528-532
- Caviggioli F, Maione L, Forcellini D, Klinger F, Klinger Autologous fat graft in postmastectomy pain syndrome. Plastic and reconstructive surgery. 2011;128:349-352
- Caviggioli F, Vinci V, Codolini Autologous fat grafting: An innovative solution for the treatment of post-mastectomy pain syndrome. Breast Cancer. 2013;20:281-282
- Salgarello M, Visconti The role of sacrolumbar fat grafting in the treatment of spinal fusion instrumentation-related chronic low back pain: A preliminary report. Spine. 2014;39:E360-E362
- Faroni A, Terenghi G, Reid Adipose-derived stem cells and nerve regeneration: Promises and pitfalls. Int Rev Neurobiol. 2013;108:121-136
- Vaienti L, Gazzola R, Villani F, Parodi Perineural fat grafting in the treatment of painful neuromas. Techniques in hand & upper extremity surgery. 2012;16:52-55
- Marangi GF, Pallara T, Cagli B, Schena E, Giurazza F, Faiella E, Zobel BB, Persichetti Treatment of early-stage pressure ulcers by using autologous adipose tissue grafts. Plastic Surgery International. 2014;2014
- Lolli P, Malleo G, Rigotti Treatment of chronic anal fissures and associated stenosis by autologous adipose tissue transplant: A pilot study. Diseases of the Colon & Rectum. 2010;53:460-466
- Cantarella G, Baracca G, Forti S, Gaffuri M, Mazzola Outcomes of structural fat grafting for paralytic and non-paralytic dysphonia. Acta Otorhinolaryngologica Italica. 2011;31:154
- DeFatta RA, DeFatta RJ, Sataloff Laryngeal lipotransfer: Review of a 14-year experience. Journal of Voice. 2013;27:512-515
- Sataloff Autologous fat implantation for vocal fold scar. Current opinion in otolaryngology & head and neck surgery. 2010;18:503-506
- Cantarella G, Mazzola RF, Mantovani M, Baracca G, Pignataro Treatment of velopharyngeal insufficiency by pharyngeal and velar fat injections. Otolaryngology– Head and Neck Surgery. 2011;145:401-403
- Papa N, Luca G, Sambataro D, Zaccara E, Maglione W, Gabrielli A, Fraticelli P, Moroncini G, Beretta L, Santaniello A. Regional implantation of autologous adipose tissue-derived cells induces a prompt healing of long-lasting indolent digital ulcers in patients with systemic sclerosis. Cell transplantation. 2014
- Hovius SE, Kan HJ, Smit X, Selles RW, Cardoso E, Khouri Extensive percutaneous aponeurotomy and lipografting: A new treatment for dupuytren disease. Plastic and reconstructive surgery. 2011;128:221-228
- Verhoekx JS, Mudera V, Walbeehm ET, Hovius Adipose-derived stem cells inhibit the contractile myofibroblast in dupuytren’s disease. Plastic and reconstructive surgery. 2013;132:1139-1148
- Bank J, Fuller SM, Henry GI, Zachary Fat grafting to the hand in patients with raynaud phenomenon: A novel therapeutic modality. Plastic and reconstructive surgery. 2014;133:1109-1118
- Damgaard OE, Siemssen Lipografted tenolysis. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2010;63:e637-e638
- Colonna M, Scarcella M, d’Alcontres F, Delia G, Lupo Should fat graft be recommended in tendon scar treatment? Considerations on three cases (two feet and a severe burned hand). European review for medical and pharmacological sciences. 2014;18:753-759
- Merikanto JE, Alhopuro S, Ritsilä Free fat transplant prevents osseous reunion of skull defects: A new approach in the treatment of craniosynostosis. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 1987;21:183-188
- Mojallal A, Lequeux C, Shipkov C, Breton P, Foyatier J-L, Braye F, Damour Improvement of skin quality after fat grafting: Clinical observation and an animal study. Plastic and reconstructive surgery. 2009;124:765-774
- Lockwood Superficial fascial system (sfs) of the trunk and extremities: A new concept. Plastic and reconstructive surgery. 1991;87:1009-1018
- Song AY, Askari M, Azemi E, Alber S, Hurwitz DJ, Marra KG, Shestak KC, Debski R, Rubin Biomechanical properties of the superficial fascial system. Aesthetic Surgery Journal. 2006;26:395-403
- Flynn The use of decellularized adipose tissue to provide an inductive microenvironment for the adipogenic differentiation of human adipose-derived stem cells. Biomaterials. 2010;31:4715-4724
- Brown BN, Freund JM, Han L, Rubin JP, Reing JE, Jeffries EM, Wolf MT, Tottey S, Barnes CA, Ratner Comparison of three methods for the derivation of a biologic scaffold composed of adipose tissue extracellular matrix. Tissue Engineering Part C: Methods. 2011;17:411-421
- Wu I, Nahas Z, Kimmerling KA, Rosson GD, Elisseeff An injectable adipose matrix for soft tissue reconstruction. Plastic and reconstructive surgery. 2012;129:1247
- Omidi E, Fuetterer L, Mousavi SR, Armstrong RC, Flynn LE, Samani Characterization and assessment of hyperelastic and elastic properties of decellularized human adipose tissues. Journal of biomechanics. 2014;47:3657-3663
- Wang L, Johnson JA, Zhang Q, Beahm Combining decellularized human adipose tissue extracellular matrix and adipose-derived stem cells for adipose tissue engineering. Acta biomaterialia. 2013;9:8921-8931
- Healy C, Allen Sr The evolution of perforator flap breast reconstruction: Twenty years after the first diep flap. Journal of reconstructive microsurgery. 2014;30:121-125
- LoTempio MM, Allen Breast reconstruction with sgap and igap flaps. Plastic and reconstructive surgery. 2010;126:393-401
- Erić M, Mihić N, Krivokuća Breast reconstruction following mastectomy; patient’s satisfaction. Acta Chir Belg. 2009;109:159-166
- Diaz-Flores L, Gutierrez R, Lizartza K, et Behavior of In Situ Human Native Adipose Tissue CD34+ Stromal/Progenitor Cells During Different Stages of Repair. Tissue-Resident CD34+ Stromal Cells as a Source of Myofibroblasts. Anatomical record. 2014.
- Gil-Ortega M, Garidou L, Barreau C, et Native adipose stromal cells egress from adipose tissue in vivo: evidence during lymph node activation. Stem cells. 2013;31(7):1309-20.
- Published in Corporate News / Blog
Scientists Confirm Reprogrammed Adult Stem Cells Identical to Embryonic Stem Cells
Click on photo (at left) to enlarge
Photo: iPS cells feature – reprogrammed stem cells: Credit: Moscow Institute of Physics and Technology
Russian researchers have concluded that reprogramming does not create differences between reprogrammed and embryonic stem cells.
Stem cells are specialized, undifferentiated cells that can divide and have the remarkable potential to develop into many different cell types in the body during early life and growth. They serve as a sort of internal repair system in many tissues, dividing essentially without limit to replenish other cells. When a stem cell divides, each new cell has the potential either to remain a stem cell or become another more specialized cell type, such as a muscle cell, a red blood cell, or a brain cell. Scientists
distinguish several types of stem cells—pluripotent stem cells can potentially produce any cell in the body. No pluripotent stem cells exist in an adult body, rather they are found naturally in
early embryos.
There are two ways to harvest pluripotent stem cells. The first is to extract them from the excess embryos produced during invitro fertilization procedures, although this practice is still ethically and technically controversial because it does destroy an embryo that could have been implanted. For this reason, researchers came up with the second way to get pluripotent stem cells— reprogramming adult cells.
Reprogramming, the process of “turning on” genes that are active in a stem cell and “turning off” genes that are responsible for cell specialization was pioneered by Shinya Yamanaka, who showed that the introduction of four specific proteins essential during early embryonic development could be used to convert adult cells into pluripotent cells. Yamanaka was awarded the 2012 Nobel Prize along with Sir John Gurdon for the discovery that mature stem cells can be reprogrammed to become pluripotent.

Production of iPS cells:
• Isolate cells from patient; grow in a dish •
Treat cells with “reprogramming”
• Wait a few weeks
• Pluripotent stem cells
• Change culture conditions to stimulate cells to differentiate into a variety of cell types
• blood cells | gut cells | cardio muscle cells
Credit: Moscow Institute of Physics and Technology
However, the extent of the similarity between induced pluripotent stem cells and human embryonic stem cells remains unclear. Recent studies highlighted significant differences between these two types of stem cells, although only a limited number of cell lines of different origins were analyzed.
Researchers compared induced pluripotent stem cell (iPSC) lines reprogrammed from adult cell types that were previously differentiated from embryonic stem cells. All these cells were isogenic, meaning they all had the same gene set.
Scientists analyzed the transcriptome – the set of all products encoded, synthesized and used in a cell. Moreover, they elicited methylated DNA areas, because methylation plays a critical role in cell specialization. Comprehensive studies of changes in the gene activity regulation mechanism showed similarities between reprogrammed and embryonic stem cells. In addition, researchers produced a list of the activity of 275 key genes that can present reprogramming results.
Researchers studied three types of adult cells – fibroblasts, retinal pigment epithelium and neural cells, all of which consist of the same gene set; but a chemical modification (e.g. methylation) combined with other changes determines which part of DNA will be used for product synthesis.
Scientists concluded that the type of adult cells that were reprogrammed and the process of reprogramming did not leave any marks. Differences between cells that did occur were thought to be the result of random factors.
“We defined the best induced pluripotent stem cells line concept,” says Dmitry Ischenko, MIPT Ph.D. and Institute of Physical Chemical Medicine researcher.
The minimum number of iPSC clones that would be enough for at least one to be similar to embryonic pluripotent cells with 95 percent confidence is five.”
 Clearly, no one is going to convert embryonic stem cells into neurons and reprogram them into induced stem cells. Such a process would be too time-consuming and expensive. This experiment simulated the reprogramming of a patient’s adult cells into induced pluripotent stem cells for further medical use, and even though the reprogramming paper, published in the journal Cell Cycle, does not currently propose a method of organ growth in vitro, it is an important step in the right direction. Both induced pluripotent cells and embryonic stem cells can help researchers understand how specialized cells develop from pluripotent cells. In the future, they may also provide an unlimited supply of replacement cells and tissues that can benefit many patients with diseases that are currently untreatable.
Clearly, no one is going to convert embryonic stem cells into neurons and reprogram them into induced stem cells. Such a process would be too time-consuming and expensive. This experiment simulated the reprogramming of a patient’s adult cells into induced pluripotent stem cells for further medical use, and even though the reprogramming paper, published in the journal Cell Cycle, does not currently propose a method of organ growth in vitro, it is an important step in the right direction. Both induced pluripotent cells and embryonic stem cells can help researchers understand how specialized cells develop from pluripotent cells. In the future, they may also provide an unlimited supply of replacement cells and tissues that can benefit many patients with diseases that are currently untreatable.The study, titled, “An integrative analysis of reprogramming in human isogenic system identified a clone selection criterion,” concluded that reprogramming does not create differences between reprogrammed and embryonic stem cells, involved researchers from the Vavilov Institute of General Genetics, Research Institute of Physical Chemical Medicine, and the Moscow Institute of Physics and Technology (MIPT).
###
- Published in Corporate News / Blog
Breakthrough in scaling up life-changing stem cell production
Scientists from the U.K. and Sweden have discovered a new method of creating human stem cells that could solve the problem of meeting large-scale production needs, allowing researchers to fully realize the potential of stem cells for understanding and treating disease.
Human pluripotent stem cells are undifferentiated cells that have the unique potential to develop into all the different types of
cells in the body. With applications in disease modeling, drug screening, regenerative medicine and tissue engineering, there is already an enormous demand for these cells, and that demand will continue grow as their use in clinical settings and the pharmaceutical industry increases.
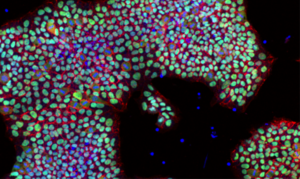
Human embryonic stem cell line HUES1 grown in the new conditions E8+Inter-alpha-inhibitor and imaged for stem cell marker Oct4 (green) and cell-cell attachment molecule E-cadherin (red) with nuclear counter-staining (blue).
Credit: Dr. Sara Pijuan-Galito and Dr. Cathy Merry, Wolfson Centre for Stem Cells, Tissue Engineering & Modelling and Centre for Biomolecular Sciences, The University of Nottingham
Read more at: http://phys.org/news/2016-07-breakthrough-scaling-life-changing-stem-cell.html#jCp
The research results, published in Nature Communications in July, describe how the scientific team from The University of Nottingham’s Wolfson Centre for Stem Cells, Tissue Engineering and Modelling at Uppsala University in Sweden and GE Healthcare also in Sweden have identified and improved human stem cell culture methods that could lead to quicker and cheaper large scale industrial production of human pluripotent stem cells.
By using a protein derived from human blood called Inter-alpha inhibitor, the team has grown human pluripotent stem cells in a minimal medium without the need for costly and time-consuming biological substrates. Inter-alpha inhibitor is found in human blood at high concentrations, and is currently a by-product of standard drug purification schemes.
The human serum-derived protein can make stem cells attach to unmodified tissue culture plastic, eliminating the need for coating in defined human pluripotent stem cell culture, and improving survival capabilities of the stem cells in harsh conditions.
It is the first stem cell culture method that does not require a pre-treated biological substrate for attachment, and therefore, is more cost and time efficient, paving the way for easier and cheaper large-scale production.
Existing methods are time consuming and make developing human stem cell cultures prohibitively costly. This new method has the potential to save time and money in large-scale and high-throughput cultures, and be highly valuable for both basic research and commercial applications.
The work began at Uppsala University, and the study’s first author, Sara Pijuan-Galitó PhD., is continuing her work as a Swedish Research Council Research Fellow at Nottingham.
Researchers now intend to combine Inter-alpha inhibitor protein with an innovative hydrogel technology to improve on current methods for controlling cell differentiation, and also apply it to disease modelling. The discovery, according to the findings, will help facilitate research into many diseases although their focus is currently on understanding rare conditions like Multiple Osteochondroma) at the cellular level. The aim is to replicate the 3 dimensional environment that cells experience within the body so that lab-bench biology is more accurate in modelling diseases.
 Pijuan-Galitó has been awarded the Sir Henry Wellcome Postdoctoral Fellowship at Nottingham University for her work on the research, which will enable her to combine Inter-alpha inhibitor with improved synthetic polymers in collaboration with fellow regenerative medicine pioneers Professor Morgan Alexander and Professor Chris Denning. The team plans to further improve on current human stem cell culture by designing an economical and safe method that can be easily translated to large-scale production and can deliver billions of stem cells necessary move cellular therapeutics forward in patient settings.
Pijuan-Galitó has been awarded the Sir Henry Wellcome Postdoctoral Fellowship at Nottingham University for her work on the research, which will enable her to combine Inter-alpha inhibitor with improved synthetic polymers in collaboration with fellow regenerative medicine pioneers Professor Morgan Alexander and Professor Chris Denning. The team plans to further improve on current human stem cell culture by designing an economical and safe method that can be easily translated to large-scale production and can deliver billions of stem cells necessary move cellular therapeutics forward in patient settings.The study, titled “Human serum-derived protein removes the need for coating in defined human pluripotent stem cell culture,” was published in Nature Communications in July, 2016.
###
- Published in Corporate News / Blog
Purest Liver-like Cells to Date Generated from Induced Pluripotent Stem Cells (iPSCs)
Researchers from the Medical University of South Carolina (MUSC) and the University of Pennsylvania have discovered a new methodology for purifying liver cells generated from induced pluripotent stem cells (iPSCs) that could facilitate progress toward an important clinical goal: treating patients with disease-causing liver mutations by transplanting unmutated liver cells derived from their own stem cells.
This new technique follows previous attempts to generate liver-like cells from stem cells, which have yielded heterogeneous cell populations with little similarity to diseased livers in patients.
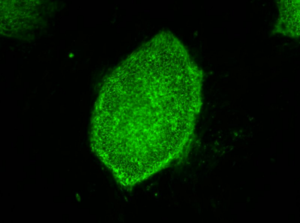
Image: induced pluripotent stem cells expressing a characteristic cell surface protein called SSEA4 (green).
Credit: Image courtesy of Stephen A. Duncan, Ph.D., at the Medical University of South Carolina
The GWAS studies map the genomes in hundreds of people as a way to look for genetic mutation patterns that differ from the genomes of healthy individuals. As GWAS study map more genomes, they become more likely to find the correct genetic mutations that cause a disease. Once a panel of suspected mutations is built, stem cells from these individuals can be manipulated in culture dishes to differentiate into any of the body’s cells. The cells can be screened to learn more about the mutations and to test panels of drugs that might ultimately help treat patients harboring a disease.
Problems arise during the cell manipulation process. For example, iPSCs persistently refuse to mature uniformly into liver-like cells when fed growth factors. Traditionally, antibodies have been used to recognize features of maturity on the surfaces of cells and purify cells that are similar, an approach that has been crucial to stem cell research. But available antibodies that recognize mature liver cells are scanty and tend to recognize many different kinds of cells. The many types of cells in mixed populations have diverse characteristics that can obscure underlying disease-causing genetic variations, which tend to be subtle.
“Without having a pure population of liver cells, it was incredibly difficult to pick up these relatively subtle differences caused by the mutations, but these differences are important in the life of an individual,” Duncan says.
Instead of relying on antibodies, Duncan and his team embraced a new technology called chemo proteomic cell surface capture (CSC) technology. CSC technology allowed the researchers to map the most highly produced proteins on the surface of liver cells during the final stages of differentiation of stem cells into liver cells. The most abundant protein was targeted with an antibody labeled with a fluorescent marker and used to sort the mature liver cells from the rest.
The procedure was highly successful: The team had a population of highly pure, homogeneous and mature liver-like cells. Labeled cells had far more similar traits of mature hepatocytes than unlabeled cells. Pluripotent stem cells that had not differentiated were excluded from the group of labeled cells.
“That’s important,” says Duncan. “If you’re wanting to transplant cells into somebody that has liver disease, you really don’t want to be transplanting pluripotent cells because pluripotent cells form tumors called teratocarcinomas.”
 Duncan cautioned that transplantation of iPSC-derived liver cells is not yet ready for translation to the clinic, but the technology for sorting homogeneous liver cells can be used now to successfully and accurately model and study disease in the cell culture dish.
Duncan cautioned that transplantation of iPSC-derived liver cells is not yet ready for translation to the clinic, but the technology for sorting homogeneous liver cells can be used now to successfully and accurately model and study disease in the cell culture dish.“We think that the ability to generate pure populations will get rid of the variability, and therefore really help us combine with GWAS studies to identify allelic variations that are causative of a disease, at least in the liver,” he says.
Researchers at the University of Minnesota (Minneapolis) and the Medical College of Wisconsin (Milwaukee) contributed to the study, published August 25, in Stem Cell Reports.
###
- Published in Corporate News / Blog
The Language of Stem Cell Medicine: What are They? What Makes Them so Special? And What do all Those Acronyms Mean?
Stem cell medicine is based on the concept that physicians can harness the body’s own reserves to heal itself, rather than relying exclusively on drugs or invasive surgical procedures. Stem cell medicine works by deals engineering human stem cells to replace or restore damaged or diseased organs or tissue, or establish normal function in them. While regenerative medicine primarily includes therapies a that utilize stem cells, the term is also used to describe therapies that use progenitor cells, used for many decades in the form of bone marrow transplants, as well as other cellular products such as platelet-rich plasma (PRP).
While both PRP and progenitor cells are widely used in clinical settings, stem cell therapies are still playing catch-up. PRP is used to treat orthopedic injuries and degenerative joint disease.
However, stem cells are in high demand worldwide. The burgeoning field of stem cell medicine is widely understood in a vague sort of way, but few people are aware that there are different kinds of stem cells. They can be derived from different tissue sources, harvested from the patient’s own body or donated. To help establish a better understanding of the stem cell landscape, we’ll start with some basic concepts.
Autologous vs. Allogenic Stem Cells
Stem cell treatments are generally divided into two classes:
- Autologous stem cells – collected from your own body, exclusively for your own use
- allogeneic stem cells, harvested from another person (donor)
Current clinical trials involving both autologous and allogeneic therapies are taking place all over the world. These trials target a wide range of diseases and conditions, from heart disease to orthopedic conditions, to wound healing.
Autologous treatments using your own stem cells can be performed in the same operative session, which eliminates concerns over your body rejecting donor cells. Your stem cells are extracted from your tissue, and reinjected back into your body targeting the area or organ that needs mending. This is a one-to-one therapy.
Allogeneic therapies use stem cells donated from another person. Before these cells can be put into a different human body than the one they came from, they must undergo extensive testing for diseases, and the cells are usually culture expanded in laboratories to achieve higher cell counts. Allogeneic therapies are performed under strict FDA guidelines, as these stem cells can eventually scale up in mass production, be stored and potentially distributed to millions of patients.
Stem Cell Types
 Adult stem cells (non-embryonic) are undifferentiated cells found throughout the body that multiply by cell division to replenish dying cells and regenerate damaged tissues.
Adult stem cells (non-embryonic) are undifferentiated cells found throughout the body that multiply by cell division to replenish dying cells and regenerate damaged tissues.
Stem cells are acquired from various tissue sources, and each tissue source has different potentials for the cells to differentiate. The following information explains these tissue sources and corresponding type of stem cells:
Adult Stem Cells (ASC’s)
In recent decades researchers discovered that stem cells can be found in all adult tissues. These are called adult stem cells, and although they cannot differentiate into every type of cell like embryonic stem cells, they can differentiate into bone, cartilage and adipose (fat) tissue readily. The two most familiar sources of adult stem cells are bone marrow and adipose tissue. More than 2,000 clinical trials have been conducted worldwide using the various tissue sources of adult stem cells.
IPS Cells (induced pluripotent cells)
IPS cells come from adult cells. Their genetic code is biologically manipulated to become pluripotent, which means they can differentiate, or become any other type of cell. Because the genetic code of IPS cells has been altered, they carry a higher risk profile than both adult stem cells and embryonic stem cells.
Embryonic Stem Cells (ES)
Embryonic stem cells, first isolated in mouse embryos in 1981, are derived from the embryo of a human fetus. Controversy has pursued embryonic stem cell research since its inception, over of ethical and religious perceptions. Embryonic stem cells are currently used mainly for research and understanding how regenerative cells work.
Types of Adult Stem Cells
Adult stem cells can be isolated from bone marrow, adipose tissue, umbilical cord blood, peripheral blood, dental pump, and  other sources. Most recently, a large number of clinical trials are focusing on stem cells derived from bone marrow and adipose tissue.
other sources. Most recently, a large number of clinical trials are focusing on stem cells derived from bone marrow and adipose tissue.
Bone Marrow Stem Cells
Bone marrow stem cells were the first recognized form of adult stem cells in the body. Researchers found they could be used to help heal bone and to replace different cell types in the blood. They could also be used in cancer patients whose bone marrow was destroyed by radiation therapy or chemotherapy. Use of bone marrow stem cells is FDA approved under certain conditions.
The drawback with bone marrow stem cells is that they are difficult to extract and not abundant. In order to be used as a treatment, bone marrow stem cells must be expanded in culture in a lab. The FDA places this therapy in the category of a drug, and requires rigorous oversight and testing.
Adipose Derived Stem Cells
In 2001, researchers and plastic surgeons from the University of Pittsburgh discovered that human fat tissue is a very rich source of mesenchymal stem cells (MSCs), multipotent stromal cells that can differentiate into a variety of cell types, and the findings were published in Tissue Engineering Journal. Upon publication, this discovery stirred quite an epiphany in the medical and scientific community—until then, adult MSCs were predominantly believed to be strictly a bone marrow product.
###
- Published in Corporate News / Blog
![RegenerativeMedicine[1]](https://stemcellcenter.net/wp-content/uploads/2018/03/RegenerativeMedicine1-460x260_c.jpg)
![WhatsApp-Image-2018-01-30-at-11.19.05-AM[1]](https://stemcellcenter.net/wp-content/uploads/2018/03/WhatsApp-Image-2018-01-30-at-11.19.05-AM1-460x260_c.jpeg)
![WhatsApp-Image-2018-01-30-at-11.17.00-AM[1]](https://stemcellcenter.net/wp-content/uploads/2018/03/WhatsApp-Image-2018-01-30-at-11.17.00-AM1-460x260_c.jpeg)
![Hair-loss-1[1]](https://stemcellcenter.net/wp-content/uploads/2018/03/Hair-loss-11-460x260_c.jpg)
![Doctor-Marketing[1]](https://stemcellcenter.net/wp-content/uploads/2018/03/Doctor-Marketing1-460x260_c.jpg)