The History of Research on Adult Stem Cells: We’ve Come a Long Way
An adult stem cell is an undifferentiated cell, found among differentiated cells in tissue or an organ. The adult stem cell can renew itself and can differentiate to yield some or all of the major specialized cell types of the tissue or organ. The primary role of adult stem cells in a living organism is to maintain and repair the tissue in which they are found. Scientists also use the term somatic stem cell to describe adult stem cells, where somatic refers to cells of the body (not the germ cells, sperm or eggs). Unlike embryonic stem cells, which are defined by their origin (cells from the preimplantation-stage embryo), the origin of adult stem cells in some mature tissues is still under investigation.
Research on adult stem cells
Research on adult stem cells has generated a great deal of excitement. Scientists have found adult stem cells in many more tissues than they once thought possible. This finding has led researchers and clinicians to consider whether adult stem cells could be used for transplants. In fact, adult hematopoietic—or blood-forming—stem cells from bone marrow have been used in transplants for more than 40 years. Scientists now have evidence that stem cells exist in the brain and the heart, two locations where adult stem cells were not at first expected to reside. If the differentiation of adult stem cells can be controlled in the laboratory, these cells may become the basis of transplantation-based therapies.
The history of research on adult stem cells began more than 60 years ago. In the 1950s, researchers discovered that the bone marrow contains at least two kinds of stem cells. Hematopoietic stem cells form all the types of blood cells in the body. Bone Marrow stromal stem cells are a multipotent subset of bone marrow stromal cells that are able to form bone, cartilage, stromal cells that support blood formation, fat, and fibrous tissue.
Types of adult stem cells
Bone marrow stem cells are also called mesenchymal stem cells, and were discovered a few years later. These non-hematopoietic stem cells make up a small proportion of the stromal cell population in the bone marrow and can generate bone, cartilage, and fat cells that support the formation of blood and fibrous connective tissue.
In the 1960s, scientists who were studying rats discovered two regions of the brain that contained dividing cells that ultimately become nerve cells, but despite these reports most scientists believed that the adult brain could not generate new nerve cells. It was not until the 1990s that scientists agreed that the adult brain does contain stem cells that are able to generate the brain’s three major cell types—astrocytes and oligodendrocytes, which are non-neuronal cells, and neurons, or nerve cells.
Where are adult stem cells found, and what do they normally do?
Adult stem cells have been identified in many organs and tissues, including brain, bone marrow, peripheral blood, blood vessels, skeletal muscle, skin, teeth, heart, gut, liver, ovarian epithelium, and testis. They are thought to reside in a specific area of each tissue (called a “stem cell niche”). In many tissues, current evidence suggests that some types of stem cells are pericytes, cells that compose the outermost layer of small blood vessels. Stem cells may remain quiescent (non-dividing) for long periods of time until they are activated by a normal need for more cells to maintain tissues, or by disease or tissue injury.
blood vessels, skeletal muscle, skin, teeth, heart, gut, liver, ovarian epithelium, and testis. They are thought to reside in a specific area of each tissue (called a “stem cell niche”). In many tissues, current evidence suggests that some types of stem cells are pericytes, cells that compose the outermost layer of small blood vessels. Stem cells may remain quiescent (non-dividing) for long periods of time until they are activated by a normal need for more cells to maintain tissues, or by disease or tissue injury.
What tests are used to identify adult stem cells?
Scientists often use one or more methods to identify adult stem cells:
• Label the cells in a living tissue with molecular markers and then determine the specialized cell types they generate;
• Remove the cells from a living animal, label them in cell culture, and transplant them back into another animal to determine whether the cells replace (or “repopulate”) their tissue of origin.
Importantly, scientists must demonstrate that a single adult stem cell can generate a line of genetically identical cells that then gives rise to all the appropriate differentiated cell types of the tissue. To confirm experimentally that a putative adult stem cell is indeed a stem cell, scientists show either that the cell can give rise to these genetically identical cells in culture, and/or that a purified population of these candidate stem cells can repopulate or reform the tissue after transplant into an animal.
- Published in Corporate News / Blog
How Clinical Trials on Stem Cell Therapies Work, and Where to Find Them
The most important resource on stem cell clinical trials is registry ClinicalTrials.gov. This registry provides the public with easy access to information on publicly and privately supported clinical studies. The ClinicalTrials.gov web site is maintained by the National Library of Medicine at the National Institutes of Health. Information (NIH) and is provided and updated by the sponsor or principal investigator of the clinical study.
Clinical Trials resources
ClinicalTrials.gov was created as a result of the Food and Drug Administration Modernization Act of 1997 (FDAMA). The site became available to the public in February 2000.
This led to the development of the ClinicalTrials.gov results database, which contains study outcomes.
Another resource, World Health Organization International (WHO) Clinical Trial Registry Platform, contains some additional information not available in the ClinicalTrials.gov registry. However, the difference is relatively small and this registry is easier to work with.
When all stem cell trials are placed on a map, we can see that vast majority of them take place in the U.S., followed by Europe.
Of the 5,101 studies, which were available on the database on August 8, 2015, 1,700 were recruiting patients and 1,769 were completed.
Clinical trials: research in human subjects
The only product that comes up as an approved treatment is Mozobil, a hematopoietic stem cell mobilizer, used in combination with granulocyte-colony stimulating factor, for the treatment of non-Hodgkin lymphoma and multiple myeloma. There are several others, such as Hemacord and Osiris, and Holoclar in Europe. This does not change the fact that approved stem cell treatments are few and far between and that is always worth checking with the relevant local regulator whether the product or treatment intervention is approved in the area or not.
Clinical research in human subjects is conducted in five phases – 0, I, II, III and IV.
• Phase 0 is an exploratory study involving very limited human exposure to the product, with no therapeutic or diagnostic goals.
• Phase 1 studies are usually conducted with healthy volunteers and emphasize safety. The goal is to find out the product’s most frequent and serious adverse events, and explore its biological effects in humans.
• Phase 2 studies gather preliminary data on effectiveness. Safety continues to be evaluated.
• Phase 3 studies gather more information about safety and effectiveness by studying different
populations and different dosages and methods of administration and by using the product in
combination with other drugs or biologics.
• Phase 4 studies occur after the approval of the product for marketing. These studies gather
additional information about a drug’s safety, efficacy, or optimal use. Not all phase 4 trials that
come up are stem cell interventions. Many of them study the effect of approved drugs and
biologics on people who received stem cell therapies.
The vast majority of these studies are in the early stages of development, and there are a considerable group of trials where the phase is not stated.
Clinical Trials: Interventional studies
The majority of stem cell research also consists of interventional studies. This means that human volunteers are assigned to interventions (for example, a medical product or procedure) based on a protocol, and are then evaluated for effects on biomedical or health outcomes.
ClinicalTrials.gov also includes records describing observational studies and programs providing access to  investigational drugs and biologics outside of clinical trials through so called expanded access.
investigational drugs and biologics outside of clinical trials through so called expanded access.
Analysis of sources of funding for stem cell trials shows only a small fraction of stem cell studies funded by the industry. A significant number of trials get funding from the National Institute of Health. All remaining trials get funding from entities categorized as “other,” meaning individuals, universities, and community-based organizations.
The sponsor of a clinical study is the organization or person who oversees the clinical study and is responsible for analyzing the study data. The funder is the organization that provides funding or support for the clinical study. Support may include providing facilities, expertise, or financial resources. Organizations listed as sponsors and collaborators for a study are considered the funders of the study.
There are four types of clinical study funders:
- National Institutes of Health
- Other U.S. Federal agency (for example, the Food and Drug Administration, Centers for Disease Control and Prevention, U.S. Department of Veterans Affairs)
- Industry (pharmaceutical and device companies)
- All others (including individuals, universities, and community-based organizations)
Although the number of studies conducted for a specific condition or disease does not tell us whether the study was successful or not, it does mean that the project was reviewed and approved as viable and that it received funding. The more studies available for a particular disease, the more accumulated knowledge exists, and the more likely it is that continuing research will yield convincing and consistent findings. On the other hand, isolated studies without posted results should be interpreted with caution.
- Published in Corporate News / Blog
What are the potential uses of human stem cells? What obstacles must still be overcome before these potential uses will be realized?
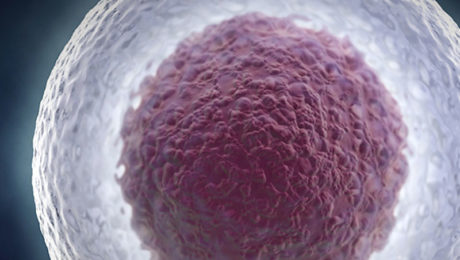
There are many ways in which human stem cells can be used in research and in the clinic. Studies of stem cells continue to yield information about their complex capabilities. A primary goal of this research is to identify how undifferentiated stem cells become the differentiated cells that form the tissues and organs. Scientists know that turning genes on and off is central to this process. Some of the most serious medical conditions, such as cancer and birth defects, are due to abnormal cell division and differentiation.
A more complete understanding of the genetic and molecular triggers of these conditions can yield information about how they arise and suggest new strategies to treat them. Predictably controlling cell proliferation and differentiation requires additional basic research on the molecular and genetic signals that regulate cell division and specialization. While recent developments with induced pluripotent stem cells (iPSCs) suggest some of the specific factors that may be involved, techniques must be developed to introduce these factors safely into the cells and control the processes that are induced by these factors.
Human stem cells and drug testing
Human stem cells are also being used to test new drugs. New medications are tested for safety on differentiated cells generated from human pluripotent cell lines. Other kinds of cell lines have a long history of being used in this way. Cancer cell lines, for example, are used to screen potential anti-tumor drugs. The availability of pluripotent stem cells would allow drug testing on a wider range of cell types. However, to screen drugs effectively, the conditions must be identical when comparing different drugs. Therefore, scientists must be able to precisely control the differentiation of stem cells into the specific cell type on which drugs will be tested.
For some cell types and tissues, current knowledge of the signals controlling differentiation falls short of being able to mimic these conditions precisely to generate pure populations of differentiated cells for each drug being tested.
Human stem cells, cell and tissue generation
Perhaps the most important potential application of human stem cells is the generation of cells and tissues that could be used for cell-based therapies. Today, donated organs and tissues are often used to replace ailing or destroyed tissue, but the need for transplantable tissues and organs far outweighs the available supply. Stem cells, directed to differentiate into specific cell types, offer the possibility of a renewable source of replacement cells and tissues to treat diseases including macular degeneration, spinal cord injury, stroke, burns, heart disease, diabetes, osteoarthritis, and rheumatoid arthritis.
used for cell-based therapies. Today, donated organs and tissues are often used to replace ailing or destroyed tissue, but the need for transplantable tissues and organs far outweighs the available supply. Stem cells, directed to differentiate into specific cell types, offer the possibility of a renewable source of replacement cells and tissues to treat diseases including macular degeneration, spinal cord injury, stroke, burns, heart disease, diabetes, osteoarthritis, and rheumatoid arthritis.
- Published in Corporate News / Blog
Mending a Broken Heart and Addressing Diabetes with Adult Stem Cells
Researchers are learning about mending a broken heart–that is, how to generate healthy heart muscle stem cells in the laboratory and then transplant those cells into patients with chronic heart disease. Preliminary research in mice and other animals indicates that bone marrow stromal cells, transplanted into a damaged heart, can have beneficial effects. Whether these cells can generate heart muscle cells or stimulate the growth of new blood vessels that repopulate the heart tissue, or help through some other mechanism is actively under investigation.
Stem Cell Research: Mending a Broken Heart
For example, injected cells may accomplish repair by secreting growth factors, rather than actually incorporating into the heart. Promising results from animal studies have served as the basis for a small number of exploratory studies in humans. Other recent studies in cell culture systems indicate that it may be possible to direct the differentiation of adult bone marrow cells into heart muscle cells.
Can Stem Cells Mend a Broken Heart? For that matter, what can stem cells do to treat all cardiovascular diseases including hypertension, coronary heart disease, stroke, and congestive heart failure? Cardiovascular disease (CVD) has ranked the number one cause of death in the United States every year since 1900 except 1918, when the nation struggled with an influenza epidemic.
Nearly 2,600 Americans die of CVD each day—roughly one person every 34 seconds. Given the country’s large aging population and the relatively dramatic recent increases in the prevalence of cardiovascular risk factors such as obesity and type 2 diabetes, CVD will be a significant health concern for decades to come.
Strategies to treat heart disease with stem cells
Cardiovascular disease can deprive heart tissue of oxygen, thereby killing cardiac muscle cells (cardiomyocytes). This loss triggers a cascade of detrimental events, including formation of scar tissue, an overload of blood flow and pressure capacity, the overstretching of viable cardiac cells attempting to sustain cardiac output leading to heart failure, and eventual death. Restoring damaged heart muscle tissue, through repair or regeneration, is therefore a potentially new strategy to treat heart failure.
The use of adult-derived stem cells for cardiac repair is an active area of research. A number of stem cell types, including cardiac stem cells that naturally reside within the heart, myoblasts (muscle stem cells), adult bone marrow-derived cells including mesenchymal cells (bone marrow-derived cells that give rise to tissues such as muscle, bone, tendons, ligaments, and adipose tissue), endothelial progenitor cells (cells that give rise to the endothelium, the interior lining of blood vessels), and umbilical cord blood cells, have been investigated as possible sources for regenerating damaged heart tissue. All have been explored in mouse or rat models, and some have been tested in larger animal models, such as pigs.
A few small studies have also been carried out in humans, usually in patients who are undergoing open-heart surgery. Several of these have demonstrated that stem cells that are injected into the circulation or directly into the injured heart tissue appear to improve cardiac function and/or induce the formation of new capillaries. The mechanism for this repair remains controversial, and the stem cells likely regenerate heart tissue through several pathways. However, the stem cell populations that have been tested in these experiments vary widely, as do the conditions of their purification and application. Although much more research is needed to assess the safety and improve the efficacy of this approach, these preliminary clinical experiments show how stem cells may one day be used to repair damaged heart tissue, thereby reducing the burden of cardiovascular disease.
Treating type I diabetes
In people who suffer from type 1 diabetes, the cells of the pancreas that normally produce insulin are destroyed by the patient’s own immune system. New studies indicate that it may be possible to direct the differentiation of human embryonic stem cells in cell culture to form insulin-producing cells that eventually could be used in transplantation therapy for persons with diabetes.
To realize the promise of novel cell-based therapies for such pervasive and debilitating diseases, scientists must be able to manipulate stem cells so that they possess the necessary characteristics for successful differentiation, transplantation, and engraftment. The following is a list of steps in successful cell-based treatments that scientists will have to learn to control to bring such treatments to the clinic. To be useful for transplant purposes, stem cells must be reproducibly made to:
- Reproduce extensively and generate sufficient quantities of cells for making tissue.
- Differentiate into the desired cell type(s).
- Survive in the recipient after transplant.
- Integrate into the surrounding tissue after transplant.
- Function appropriately for the duration of the recipient’s life.
- Avoid harming the recipient in any way.
Also, to avoid the problem of immune rejection, scientists are achieving good results with strategies that use the patient’s own stem cells to generate tissue that will not be rejected.
- Published in Corporate News / Blog
Stem Cell Research and Stem Cell Therapy: When can stem cells be used to treat patients?
The difference between stem cell research and therapy is in the scientific evidence that supports therapeutic intervention to be beneficial for the patient.
Stem cells have the remarkable potential to develop into many different types of cells in the body during early life and growth. In addition, in many tissues, stem cells serve as a sort of internal repair system, dividing essentially without limit to replenish other cells as long as the individual is alive. When a stem cell divides, each new cell has the potential either to remain a stem cell or become another type of cell with a more specialized function, such as a muscle cell, a red blood cell, or a brain cell.
Stem cell research on adult stem cells
Stem cells are distinguished from other cell types by two important characteristics. First, they are unspecialized cells capable of renewing themselves through cell division, sometimes after long periods of inactivity. Second, under certain physiologic or experimental conditions, they can be induced to become tissue- or organ-specific cells with special functions. In some organs, such as the gut and bone marrow, stem cells regularly divide to repair and replace worn out or damaged tissues. In other organs, such as the pancreas and the heart, stem cells only divide under special conditions.
Until recently, scientists primarily worked with two kinds of stem cells from animals and humans: embryonic stem cells and non-embryonic “somatic” or “adult” stem cells in stem cell research.
In 2006, researchers made a breakthrough by identifying conditions that would allow some specialized adult cells to be “reprogrammed” genetically to assume a stem cell-like state. This new type of stem cell is called induced pluripotent stem cells (iPSCs).
Stem cells are important for living organisms for many reasons. In the 3- to 5-day-old embryo, called a blastocyst, the inner cells give rise to the entire body of the organism, including all of the many specialized cell types and organs such as the heart, lungs, skin, sperm, eggs and other tissues. In some adult tissues, such as bone marrow, muscle, and brain, discrete populations of adult stem cells generate replacements for cells that are lost through normal wear and tear, injury, or disease.
Stem cell research for treating disease
Given their unique regenerative abilities, stem cells offer new potentials for treating diseases such as diabetes, and heart disease. However, much work remains to be done in the laboratory and the clinic to understand how to use these cells for cell-based therapies to treat disease, which is also referred to as regenerative or reparative medicine.
Laboratory studies of stem cells enable scientists to learn about the cells’ essential properties and what makes them different from specialized cell types. Scientists are already using stem cells in the laboratory to screen new drugs and to develop model systems to study normal growth and identify the causes of birth defects.
Research on stem cells continues to advance knowledge about how an organism develops from a single cell and how healthy cells replace damaged cells in adult organisms. Stem cell research is one of the most fascinating areas of contemporary biology, but, as with many expanding fields of scientific inquiry, research on stem cells raises scientific questions as rapidly as it generates new discoveries.
In 1964, the World Medical Association developed the Declaration of Helsinki as a statement of
ethical principles for medical research involving human subjects. It includes research on identifiable human material and data, last amended in October 2013.
According to the Helsinki Declaration, in the treatment of an individual patient where proven interventions do not exist or other known interventions have been ineffective, the physician, after seeking expert advice, with informed consent from the patient or a legally authorized representative, may use an unproven intervention if in the physician’s judgement it offers hope of saving life, re-establishing health or alleviating suffering.
Intervention should subsequently be made the object of research, designed to evaluate its safety and efficacy. In all cases, new information must be recorded and, where appropriate, made publicly available.
- Published in Corporate News / Blog
Stem Cell Myths, Busted
The term stem cell research gleans different reactions from people, both in the medical community and the wider public. Still an emerging science, stem cell research is shrouded by many myths and misconceptions. Here, we take on some of the most predominant myths to discuss the misconceptions and clarify the facts regarding this fast-growing branch of medicine.
Stem cell myths
Myth #1: Stem cells only come from embryos.
FACT: False. Stem cells exist in all bodies, from embryos to adults.
Embryonic stem cells come from the early embryo, and have the potential to produce all the specialized cells of the body. Because of this, they hold great promise for studying and potentially treating disease and injuries. Tissue or “adult” stem cells are found in the body throughout our lives. These cells maintain and repair many tissues in the body. Examples of these cells include blood stem cells, muscle stem cells, bone marrow stem cells, adipose tissue (fat) stem cells and skin stem cells. Some of these adult stem cells are used in established medical and aesthetic treatments.
Myth #2: Induced pluripotent stem cells (iPSCs) eliminate the need for embryonic cells
FACT: False. Research is needed on all types of cells because it is not clear which cells will be most useful for which types of application. For the foreseeable future, side-by-side research on both embryonic and induced pluripotent stem cells is needed. Global Stem Cell Group’s research and treatment products use no embryonic stem cells.
Myth #3: Stem cell research leads to cloning humans.
FACT: False. Most countries prohibit this type of cloning.
In most countries, even attempting to clone a human being is illegal. Some countries do allow something called “therapeutic cloning” for the purposes of studying a disease. In this procedure, scientists isolate embryonic stem cells from a cloned blastocyst (early stage embryo) but do not transfer the blastocyst into a womb. In therapeutic cloning, the blastocyst is not transferred to a womb. Instead, embryonic stem cells are isolated from the cloned blastocyst. These stem cells are genetically matched to the donor organism for studying genetic disease. For example, stem cells could be generated using the nuclear transfer process described above, with the donor adult cell coming from a patient with diabetes or Alzheimer’s. The stem cells could be studied in the laboratory to help researchers understand what goes wrong in diseases like these.
Therapeutic cloning also could be used to generate cells that are genetically identical to a patient’s. A patient transplanted with these cells would not suffer the problems associated with transplant rejection. To date, no human embryonic stem cell lines have been derived using therapeutic cloning.
Myth #4: Adult stem cells are only found in adults
FACT: False. There are three different types of stem cells: embryonic stem cells, induced pluripotent stem cells and tissue specific stem cells. It’s the tissue stem cells that are often called “adult” stem cells, but these “adult” stem cells are found in people of all ages. (See myth #1).
Stem cell myths: research
Myth #5: Embryonic stem cell research is banned in Europe.
FACT: False. The laws vary across the EU.
EU member states have diverging regulatory positions on human embryonic stem cell research. For instance, in Germany, the use of embryos for research is heavily restricted under the Embryo Protection Act (Embryonenschutzgesetz) of 1991, which makes the derivation
of embryonic stem cell lines a criminal offense. But in the UK, embryonic stem cell research is allowed, subject to licensing from the Human Fertilization and Embryology Authority (HFEA). Click here for country by country overviews for more details. Under the previous two European Framework programs (FP6 and F7), as well as the current program, Horizon 2020, human embryonic stem cell research can be funded, provided that the work is permitted by law in the country where it is to take place.
Myth #6: Stem cell research and treatment is against the law in the US.
FACT: False. The FDA does not regulate the practice of medicine, but rather drugs and medical devices and which of these can be marketed in the US. Under federal law, cultured (grown) stem cell products are considered a drug, but are not illegal. Adult stem cells, however, are not cultured—they exist in our bodies throughout our organs, blood, skin, teeth, fat, bone marrow and other places.
Adult stem cell therapy is currently used in the United States to treat conditions such as leukemia and other illnesses. Bone marrow consists of stem cells which have been transplanted for years in the US.
Global Stem Cells Group offers stem cell treatments in countries where stem cell therapy is approved and regulated with no appreciable difference in safety record.. Stem cell therapy technology is still under review by the FDA.
Stem cell myths: therapies
Myth #7: Bone marrow is the best source of stem cells.
FACT: False. Bone marrow is just one source of stem cells. Bone marrow stem cells have been studied for decades, and have been used to treat certain types of cancer. A great deal of research has been dedicated to understanding this source of stem cells and their potential. Bone marrow contains a number of different kinds of stem cells, one of which is mesenchymal stem cells. However, mesanchymal stem cells can also be found in adipose (fat) tissue at nearly 2000 times the frequency of bone marrow.
Mesenchymal cells have the capability to become different types of tissues (blood vessels, muscle tissue, etc.) and are capable of communicating with other cells. In combination with other proteins, molecules and regenerative cells found in adipose tissue, they also have the ability to reduce inflammation, regenerate damaged tissue, and grow new blood vessels, a process known as angiogenesis. Stem cells from adipose tissue are more accessible and abundant. They can be processed immediately and reintroduced into the body right away.
Myth #8: There is a risk of rejection with stem cell therapy.
FACT: False. When a patient’s stem cells are derived from his or her own body (such as fat tissue), there is no risk of rejection. In fact, studies thus far have indicated no safety issues with fat-derived autologous (from self) stem cells. Since these stem cells come from your own body, the risk of rejection is eliminated.
###
- Published in Corporate News / Blog
Gordie Howe’s Stem Cells Treatments Support a Growing Appeal for These Therapies Among Athletes and Baby Boomers
In October, 2014, legendary hockey player Gordie Howe, then 86, was on death’s door after suffering a debilitating acute hemorrhagic, left thalamus stroke. Upon returning home from the hospital, Howe needed someone to lift him from his bed to a wheelchair and back. He couldn’t remember the names of his four children, Marty, Mark, Cathy, and Murray, and his condition continued to grow worse in subsequent weeks. According to an article in New York Magazine, when Mark took his father to get an epidural to relieve his back pain, the attending physician took one look at Gordie and asked Mark if it might be better to just let his father go. On the rare occasion when Gordie did manage to speak, he would tell his children, “Just take me out back and shoot me.”
The man for whom the term “hat trick” was coined, Howe retired from hockey at age 52 after four decades of professional play, having scored more goals than any other NHL player. But over the past 10 years, his health declined dramatically—heart disease, dementia, and spinal stenosis—despite his family’s and physician’s best efforts to find medical solutions. After his stroke, Keith Olbermann aired a preemptive obituary on ESPN. The family made funeral plans. Murray, his youngest son, wrote a eulogy.
Experimental stem cell treatment
Around Thanksgiving, 2015, Howe’s family learned about an experimental stem cell treatment that could save his life. The plan was to inject up to 100 million neural stem cells into his spinal column in the hopes that the stem cells would migrate to his brain and help his body repair itself. Howe could improve within 24 hours, and receive the treatment anytime—just not in the United States. The procedure wasn’t FDA-approved, and Howe would have to receive the treatment at a clinic in Tijuana.
Howe’s son Murray, a radiologist, looked into the treatment and thought it was promising. The real concern was transporting the immobile Howe to Mexico. Daughter Cathy worried that he might die during the treatment, but Mark responded bluntly: “If he does die, what’s the difference? He’s going to be gone soon no matter what.”
While the family weighed the stem cell treatment idea, Howe was admitted to the hospital with severe dehydration, caused by his unwillingness to swallow. When he returned home, he still had no use of his right side, and the family assumed he would never walk again. The Howe children decided to give the stem cell treatments a try.
Two days later, the Howes flew their Dad to San Diego. In the air, Gordie grew agitated and got the attention of a flight attendant, who spent 10 minutes kneeling by his seat trying to understand something he wanted to tell her. Due to his profound memory loss, Howe didn’t know he had suffered a stroke, why he was on a plane, or where he was going. But he remembered one thing, which he managed to whisper to the fight attendant: “I was a pro hockey player.”
The next morning, Marty and Murray drove with their father across the border to Clínica Santa Clarita, where Gordie bent over a table to expose his lower back so that a needle could be inserted into his spinal canal to inject the stem cells. Howe was given two types of stem cells – neural stem cells and mesenchymal stem cells. The second type, derived from bone marrow, has anti-inflammatory properties and secretes chemicals that promote healing.
The procedure then required Howe to lie prone for eight hours. After the eight hours passed, Gordie told Murray he needed to use the bathroom and that he intended to walk there in order to do so. Since the stroke, Gordie had only managed to walk one time—10 steps, with a walker. Murray reminded his Dad that he couldn’t walk.
Recovery milestone after stem cell treatment
Howe stood up, and with Murray’s support, walked for the first time in more than a month—to the bathroom. This milestone became an oft-repeated story among the Howe family, and Gordie’s revival became an irresistible story for the sports pages. Back home, Gordie returned to something resembling the normal life of an 86-year-old. He pushed the grocery cart, helped with the dishes, and could go fishing so long as one of his sons reminded him that a tug on the line meant he needed to start reeling. The family released a video of Gordie standing stationary, firing a puck, five-hole, past his 8-year-old great-grandson. Keith Olbermann apologized for his premature obituary.
Howe’s children now had to figure out how to share his apparent recovery—a debate that proved just as contentious as their decision to fly him to Mexico for the treatment in the first place—with the world. Both Marty and Mark had played in the NHL alongside their father, but now Murray, the doctor, was giving interviews in his hospital scrubs, endorsing his father’s place in medical “miracle” history. He began referring to the stem-cell treatment as the “Gordie Howe Protocol,” and said that his Toledo-based hospital was looking into conducting an FDA-approved study of the procedure. In one interview, Murray Howe stated that “stem cells are the most promising thing in medicine since the discovery of antibiotics.”
As the story spread, the medical community started to question just how miraculous Howe’s recovery had been.
“Companies selling these products are preying on desperate and vulnerable people and exploiting their hope, much like snake-oil salesmen have done throughout most of human history,” wrote Judy Illes and Fabio Rossi, stem-cell experts at the University of British Columbia, in the Vancouver Sun. Even advocates pointed out that, though the field holds great promise, no reputable studies have shown that such a procedure should work.
And yet, for the children of ailing parents, such skepticism doesn’t matter. Murray’s response to one skeptic was, “What would you do for your father?”
Gordie Howe’s therapy would cost an average patient about $30,000.
Athletes, whether playing or retired, have a special need for the regenerative capacity that stem cells are believed to provide. Athletes break bones, strain ligaments, bash knees and wear out cartilage. If stem cells’ restorative capability is proven, they could be considered the latest form of sports medicine.
Since Howe’s treatment in late 2014, two other athletic legends have received stem cell treatments—former quarterbacks Bart Starr and John Brodie. And the rest of the population, particularly aging baby boomers, isn’t far behind.
 Still, while acceptance of stem cell therapy has grown, so have controversies surrounding its use. While clinical trials authorized by the U.S. Food and Drug Administration are rapidly expanding in the U.S., so are treatments outside the regulated system. Patients are going to stem cell clinics in other countries that approve stem cell therapies.
Still, while acceptance of stem cell therapy has grown, so have controversies surrounding its use. While clinical trials authorized by the U.S. Food and Drug Administration are rapidly expanding in the U.S., so are treatments outside the regulated system. Patients are going to stem cell clinics in other countries that approve stem cell therapies.
For its part, the FDA is drafting guidelines, although the U.S. and Canada still trail other countries in approving stem cell treatments.
Last year, the FDA issued draft guidelines to clarify what types of human cell therapy it regulates. The short answer: Most of them, with “limited exceptions,” according to an FDA email sent in response to questions from The San Diego Union-Tribune. These exceptions include cells or tissues that are “minimally manipulated,” not given with any other product and perform the same function in the donor as in the recipient.
All other stem cell therapies are seen as involving human cells, tissues and cellular and tissue-based products – also known as HCT/Ps – regulated by the FDA’s Center for Biologics Evaluation and Research.
“We understand that determining the appropriate regulatory path for HCT/Ps can be challenging, and the FDA is working diligently to develop guidance to help sponsors and physicians understand how to apply federal regulations to this complex and emerging field,” the agency said.
In January 2015, University of California, Davis stem cell researcher and blogger Paul Knoepfler estimated that more than 100 unauthorized stem cell clinics were operating in the United States. Later that year, he increased that estimate to up to 200.
Then on May 6, he wrote in his blog: “We are seeing a flood of professional athletes getting stem cell treatments in the past few years.”
Athletes and others who want these treatments bristle at what they call cumbersome, time-consuming regulations in the U.S. The situation can be urgent for seriously ill patients.
While it hasn’t been proven that the stem cells enabled his recovery, by all indications Gordie Howe’s health has improved significantly since receiving stem cell treatments. In November, 2015, Murray Howe said that his father’s physicians in the U.S. recommended hospice care in the weeks after the stroke, and the family was told he wouldn’t last more than two or three weeks,
“Then, suddenly, he is raking and sweeping and goofing around in the back yard,” Murray said.
###
###
Sources: The San Diego Union-Tribune, New York Magazine
- Published in Corporate News / Blog
Stem Cell Researchers Discover Stem Cells That Might Repair Skull, Face Bones
Scientists may be one step closer to a breakthrough that uses stem cells to replace damaged skull and facial bones in patients who experience a head trauma or undergo cancer surgery requiring repair and reconstructive surgery.
Researchers have discovered and isolated stem cells capable of repairing these bones in mice. The research, led by Takamitsu Maruyama and the research team at the University of Rochester Medical Center in Rochester, N.Y., could also help patients born with a skull deformity known as craniosynostosis, which can lead to developmental delays and pressure on the brain.
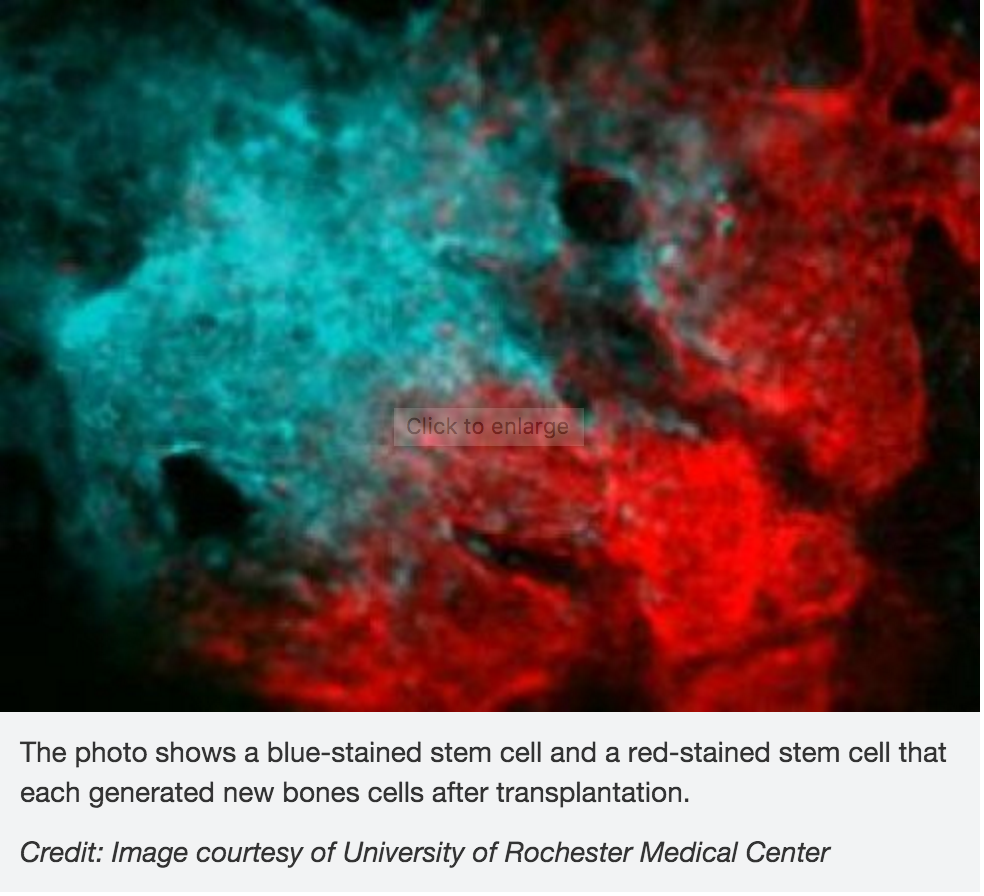 In the study, scientists investigated the role of the Axin2 gene in bone formation and regeneration. They also examined a specific mutation that causes craniosynostosis in mice. Their finding show that stem cells involved in skull formation are contained within this cell population. These cells are specificto the bones in the head and are very different from other stem cells involved in the formation of the bones in the legs and other parts of the body.
In the study, scientists investigated the role of the Axin2 gene in bone formation and regeneration. They also examined a specific mutation that causes craniosynostosis in mice. Their finding show that stem cells involved in skull formation are contained within this cell population. These cells are specificto the bones in the head and are very different from other stem cells involved in the formation of the bones in the legs and other parts of the body.
Tests to uncover these cells could also help physicians detect bone diseases caused by stem cell abnormalities, according to the researchers.
The research was published Feb. 1 in the journal Nature Communications.
- Published in Corporate News / Blog
German Stem Cell Scientists Develop 3-D “Mini-retinas” –New Hope for Restoring Sight in Patients with Retinal Degeneration Caused by Diabetes and Inherited Disorders.
Medical breakthroughs using stem cells are aimed at all parts of the body bones, kidneys, joints, spines–and now, sight.
A German study in March in Stem Cell Reports, reports that scientists have created an efficient way of developing 3D retina organoids leverage the self-organizing properties of stem cells to create diverse multi-cellular tissue proxies.
3-D Mini-retinas protocol
The new mini-retina protocol involves cutting an organoid grown from stem cells into three, half-moon shaped pieces at an early stage of eye development. Each of these pieces eventually grows into the full suite of cells found in the retina.
3-D retinal organoids developed in this process efficiently replicate retina formation. This includes the light-detecting cone cells, which now can be produced in high quantities.
cone cells, which now can be produced in high quantities.
Cone photoreceptors, which are responsible for high acuity and color vision, are the most precious retinal cell type with regard to potential future cell replacement therapies in patients affected by retinal degeneration caused by diabetes and inherited disorders.
The process of developing 3D retinal organoids also allows the surviving organoids to grow to reach sizes similar to uncut organoids. These mini-retinas swim around in the dish and because they’re not attached to a surface, better reflect the structure of retinal tissue during development.
In the past, the inability to produce such cells has been a major limitation for regenerative medicine; however, this new method increases the yield of retinal organoids 4-fold, allowing researchers to take a great step forward in the study of the retina and how to repair it.
3-D Mini-retinas offer more diverse ways to study retina tissue
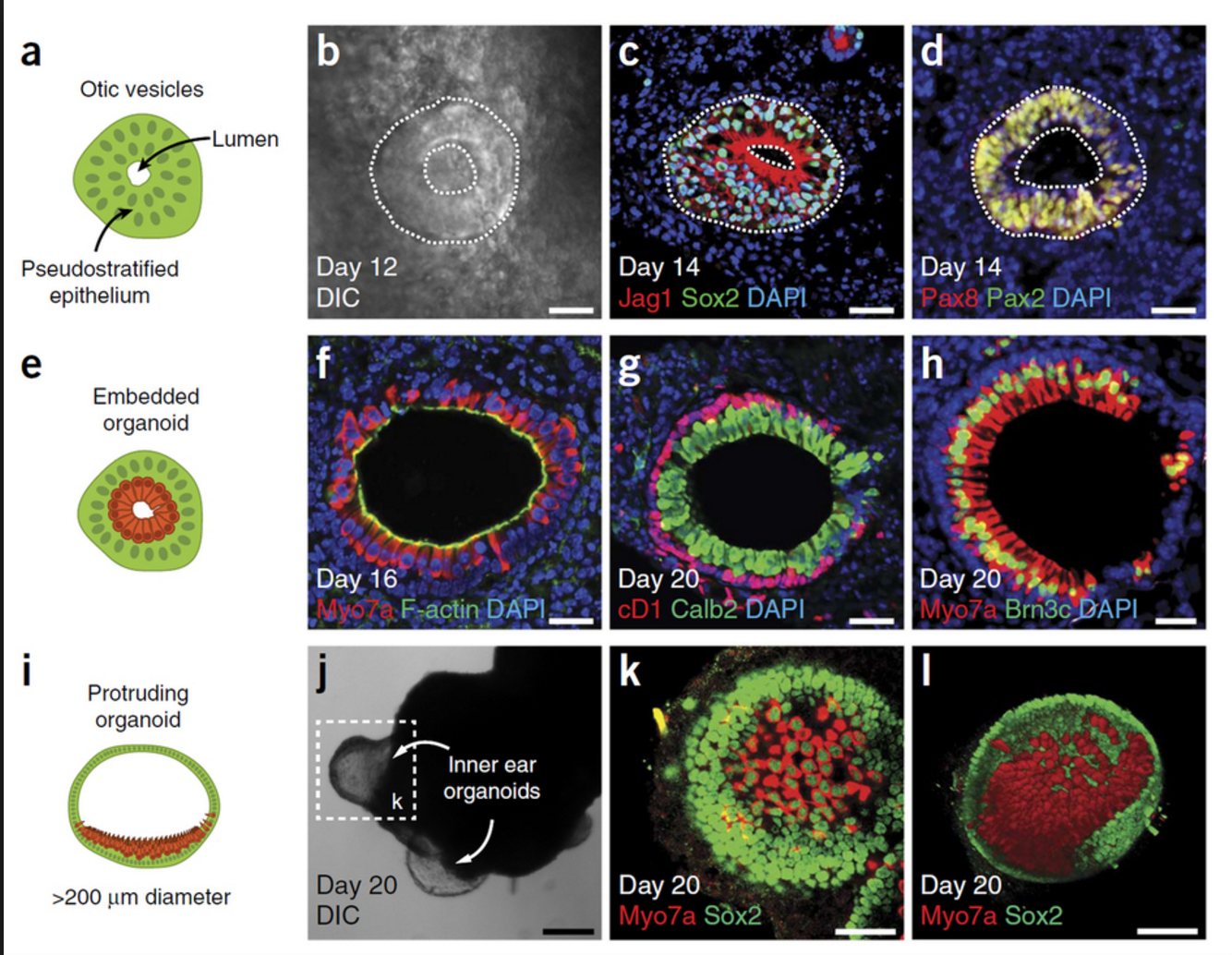 “The goal isn’t just to make the closest thing next to a real retina, but also to possibly harness the flexibility of the system to create more diverse ways of studying retina tissue,” says senior author Mike Karl, of the German Center for Neurodegenerative Diseases (DZNE) and part of the Center for Regenerative Therapies (CRTD) at Technische Universität Dresden.
“The goal isn’t just to make the closest thing next to a real retina, but also to possibly harness the flexibility of the system to create more diverse ways of studying retina tissue,” says senior author Mike Karl, of the German Center for Neurodegenerative Diseases (DZNE) and part of the Center for Regenerative Therapies (CRTD) at Technische Universität Dresden.
“Even with our new additions to existing organoid systems, we have not yet reached that tipping point of robustness that we need for people without the expertise to grow these models.”
Karl and his colleagues’ comparative studies on pluripotent stem cell-derived human and mouse retina organoids and mouse retina in vivo support the power of the new organoid protocol.
New insights in the study of retinal disease
“Tissue heterogeneity (diversity) is a major challenge in organoid systems, and here our work provides new insight, which will help to develop specific organoid-based models, specifically to reliably study retinal disease mechanism,” says Karl.
The Karl Lab’s change to the mini-retina protocol involves cutting a retina organoid grown from stem cells into three pieces at an early stage of eye development. Each of these pieces, which look like little half moons, eventually grows into the full suite of cells found in the retina, thereby increasing the yield of retinal organoids up to 4-fold compared to previous protocols. Karl’s next objective is to make his 3-D “mini-retinas” even more complex, perhaps by bringing in blood vessels and using the organoids to study regeneration and the function of different neural cell types–specifically, from the human retina.
- Published in Corporate News / Blog
Stem Cell Treatments Normally Used for Cancer Patients are Helping Multiple Sclerosis Patients
The British Broadcasting Corporation (BBC) recently reported that stem cell transplant treatments normally used for cancer patients are helping Multiple Sclerosis (MS) patients in the UK. According to the January 18, 2016 report, 20 patients received bone marrow stem cell transplants using their own stem cells, and that at least some of the patients who were paralyzed by MS are able to walk again post-treatment.
Approximately100,000 people in the United Kingdom suffer from MS, with most new patients diagnosed between the ages of 20 and 30 years of age.
“To have a treatment which can potentially reverse disability is really a major achievement,” says Prof Basil Sharrack, of Sheffield’s Royal Hallamshire Hospital in Sheffield, England.
The treatment, known as autologous hematopoietic stem cell transplantation (HSCT), involves the intravenous infusion of autologous or allogeneic stem cells harvested from the patient’s own bone marrow to reestablish hematopoietic function (formation of blood or blood cells) in patients whose bone marrow or immune system is damaged or defective by chemotherapy. Using stem cells harvested from the patient’s bone marrow helps rebuild the immune system. The theory is that these newly harvested cells are at such an early stage in development that the cellular defects that result in MS do not exist.
“The immune system is being reset or rebooted back to a time point before it caused MS,” says Prof John Snowden, consultant hematologist at Royal Hallamshire Hospital.
The BBC’s Panorama program spoke to several MS patients who have undergone the stem cell transplant.
Steven Storey was diagnosed with MS in 2013 and, within a year, went from being an able-bodied athlete to wheelchair dependent and losing sensation in much of his body.
“I went from running marathons to needing 24-hour acute care. At one point I couldn’t even hold a spoon and feed myself,” Storey says.
Within a few days of the transplant Storey was able to move his toes, and after four months he could stand unaided.
While Storey still needs a wheelchair for mobility, he calls his progress astounding.
“It’s been incredible,” he says. “I was in a dire place, but now I can swim and cycle and I am determined to walk.”
The Royal Hallamshire Hospital along with hospitals in the United States, Sweden and Brazil, is part of an international clinical trial called MIST that is assessing the long-term benefits of the stem cell procedure on MS patients. Study participants all have relapsing remitting MS (RRMS), and received intensive chemotherapy to completely destroy the patients’ immune systems.
Treatment costs are about the same as the annual cost for existing treatments, and the stem cell treatment does not require the use of new or existing medications.
Prof Richard Burt of Northwestern University in Chicago carried out the first hematopoietic stem cell transplantation for MS in 1995, and is coordinating this current MIST international trial, which began in 2006.
“There has been resistance to this in the pharma and academic world,” Burt says. “This is not a technology you can patent and we have achieved this without industry backing.”
A study published last year involving MS patients in Chicago showed significant reductions in neurological disability, and for some the improvements persisted for at least four years, although there was no comparative control group.
The outcomes of the current international trial will be reported in 2018, and may determine whether the stem cell transplant becomes a standard in the United Kingdoms health care system for many MS patients.
“Ongoing research suggests stem cell treatments such as HSCT could offer hope, and it’s clear that in the cases highlighted by Panorama they’ve had a life-changing impact,” says Emma Gray, M.D., head of clinical trials at UK’s MS Society.
- Published in Corporate News / Blog